Anecdotally have heard initial TORS experience in HN at many institutions had lots of severe complications: major bleeding, trachs, deaths. ECOG 3311 wouldn't let surgeon on without a solid prior case log, and would throw surgeons off trial if too many + margins.Is this fundamentally different than rare, extreme complications in the hands of inexperienced users with other new devices in other interventional specialties? Honestly asking because I don't know.
As someone who does SpaceOAR in the office fairly often myself (and have not personally seen these complications), I feel very, very comfortable doing it and offering it to patients but would certainly want SpaceOAR by someone with experience if it was for myself or a family member.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
SpaceOAR - Augmenix, Boston Scientific, and Conflicts of Interest
- Thread starter elementaryschooleconomics
- Start date
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
Yip. Saw lots of a trismus.Anecdotally have heard initial TORS experience in HN at many institutions had lots of severe complications: major bleeding, trachs, deaths. ECOG 3311 wouldn't let surgeon on without a solid prior case log, and would throw surgeons off trial if too many + margins.
- Joined
- Aug 4, 2020
- Messages
- 1,967
- Reaction score
- 3,354
68/25 and no spacer gel. If they have a huge prostate and/or modest prostate with significant AUA, then conventional.Did you hack my EMR
But seriously, there is some data that fiducials provide lower systematic error. On paper this allows a tighter PTV by margin recipes. In real life, it very well not matter at all. There is probably a lot of “pseudoPTV” by calling the entire prostate gland the CTV.
I'd consider spacer for SBRT, but I ain't doin SBRT for prostate.
Patients are instructed to come in "the middle" ie not bursting and not empty.. ie the same way they get sim'd. CBCT every day, and experienced therapists line it up or call if it doesn't look right.
Other than a couple immodium occasionally, I haven't seen any big issues and most patients have none...
I see no value to use it, other then the answer to "why are you using the gel?" Because all of life's why questions have the same answer.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
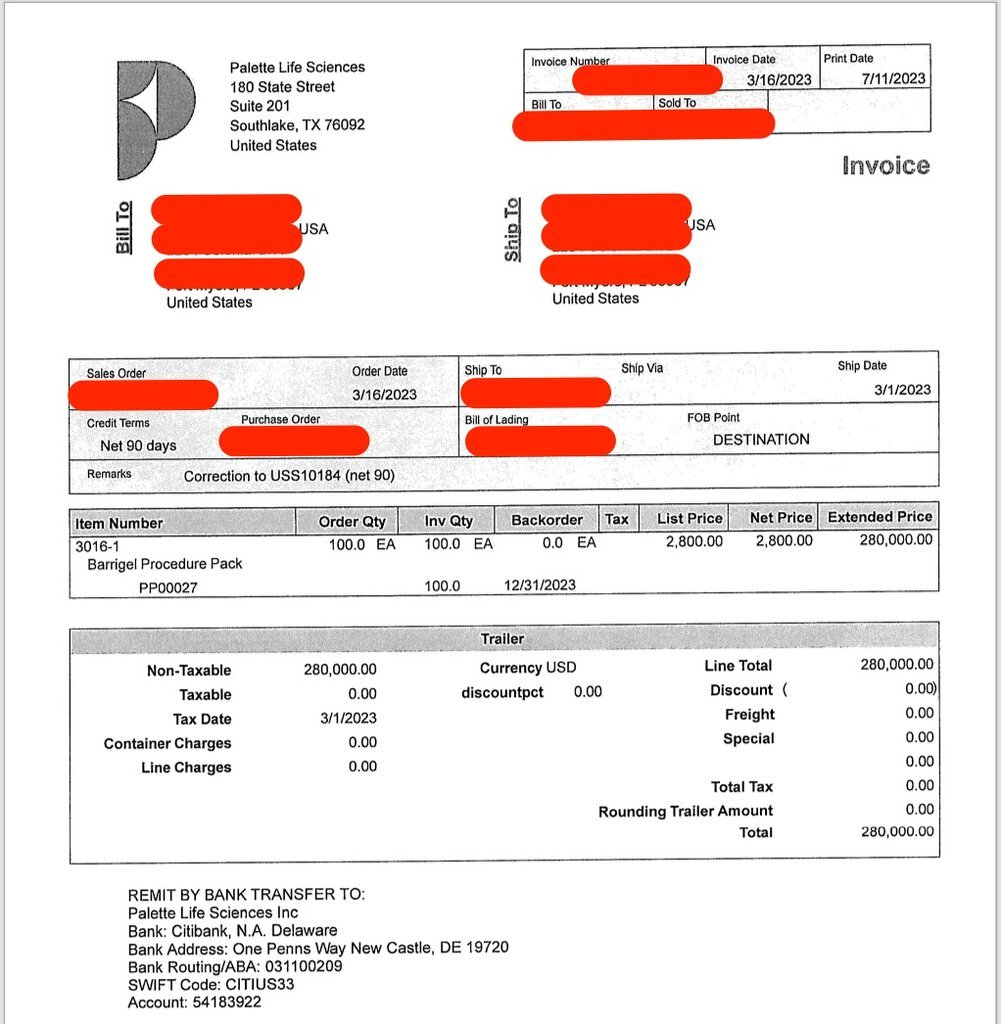
$280K for ? benefit:
- Joined
- Aug 4, 2020
- Messages
- 1,967
- Reaction score
- 3,354
Actual cost?
Gel is cheap. Regulations are expensive. Markup is insane.
Welcome to the medical world.
Gel is cheap. Regulations are expensive. Markup is insane.
Welcome to the medical world.
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
I don’t u
I don’t understand this?Actual cost?
Gel is cheap. Regulations are expensive. Markup is insane.
Welcome to the medical world.
- Joined
- Apr 3, 2019
- Messages
- 4,269
- Reaction score
- 9,961
$2800 per “squirt” in other words. Remember that 80s heavy metal song Cum On Feel the Noize?
- Joined
- Apr 3, 2019
- Messages
- 4,269
- Reaction score
- 9,961
I think he’s saying $2800 is a lot to pay for the molecular (makeup, and moles) equivalent of a 10 dollar can of AXE hair pomade. And the pomade is crazily marked up itself.I don’t u
I don’t understand this?
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
From the ACS website forum
“
Spaceoar didn't protect
My dad had the spaceoar done in December of 2018 and he ended up doing five rounds of Radiation therapy, after the last dose of radiation he began having issues he had a anal uretha fistula he suffered for months then had to have emergency surgery his bladder, prostate and rectum had to be removed he almost bled to death. The radiation oncologist said the Spaceoar caused and unusual inflammatory response in my dad's body and radiation made it worse. If anyone is on the fence about whether or not to get the Spaceoar or not please due your research, my dad's life has changed forever. “

 csn.cancer.org
csn.cancer.org
“
Spaceoar didn't protect
My dad had the spaceoar done in December of 2018 and he ended up doing five rounds of Radiation therapy, after the last dose of radiation he began having issues he had a anal uretha fistula he suffered for months then had to have emergency surgery his bladder, prostate and rectum had to be removed he almost bled to death. The radiation oncologist said the Spaceoar caused and unusual inflammatory response in my dad's body and radiation made it worse. If anyone is on the fence about whether or not to get the Spaceoar or not please due your research, my dad's life has changed forever. “

SpaceOAR gel
Has anyone had a bad experience with SpaceOAR gel? I had the procedure on Thursday and the pain is still there today.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
And…
“Needless to say I'm updet to
Needless to say I'm updet to the point about thinking lawsuit then again I don't want bad karma”
“Needless to say I'm updet to
Needless to say I'm updet to the point about thinking lawsuit then again I don't want bad karma”
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
And…
“I had SpaceOAR gel inserted on 7/13/22. I constantly had the feeling of needing to have a bowl movement & bleeding, along with mucus. After about 3 weeks of this they sent me for another MRI & said that the hydrogel had penetrated my rectal wall. I've been dealing with pain, pressure, rectal urgency & bleeding for over 2 months. The Dr. says that I should get some relief after the 90 day mark of the procedure. Has anyone else had to deal with this?”
“I had SpaceOAR gel inserted on 7/13/22. I constantly had the feeling of needing to have a bowl movement & bleeding, along with mucus. After about 3 weeks of this they sent me for another MRI & said that the hydrogel had penetrated my rectal wall. I've been dealing with pain, pressure, rectal urgency & bleeding for over 2 months. The Dr. says that I should get some relief after the 90 day mark of the procedure. Has anyone else had to deal with this?”
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
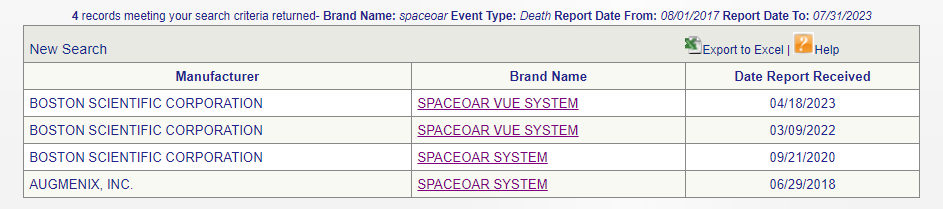
I also did a cursory review of the MAUDE website and fistulas continue to be reported.
D
deleted1111261
Should their be prior auth for spacers? There currently is not for most payors
- Joined
- Dec 29, 2014
- Messages
- 339
- Reaction score
- 613
In what cases would you consider it justifiable.Should their be prior auth for spacers? There currently is not for most payors
Feels like there are believers and non believers. Not sure what decision rules you'd use as a non believer to justify it.
- Joined
- Sep 20, 2004
- Messages
- 11,747
- Reaction score
- 11,839
Different pt than the one published by UTSW? 2 guys with pelvic exents now. InsaneFrom the ACS website forum
“
Spaceoar didn't protect
My dad had the spaceoar done in December of 2018 and he ended up doing five rounds of Radiation therapy, after the last dose of radiation he began having issues he had a anal uretha fistula he suffered for months then had to have emergency surgery his bladder, prostate and rectum had to be removed he almost bled to death. The radiation oncologist said the Spaceoar caused and unusual inflammatory response in my dad's body and radiation made it worse. If anyone is on the fence about whether or not to get the Spaceoar or not please due your research, my dad's life has changed forever. “

SpaceOAR gel
Has anyone had a bad experience with SpaceOAR gel? I had the procedure on Thursday and the pain is still there today.csn.cancer.org
- Joined
- Jun 3, 2021
- Messages
- 20
- Reaction score
- 59
Nothing like trying to reduce the <5% risk of a G3 or greater toxicity by starting with a definite G3 or > toxicity.“I had SpaceOAR gel inserted on 7/13/22. I constantly had the feeling of needing to have a bowl movement & bleeding, along with mucus. After about 3 weeks of this they sent me for another MRI & said that the hydrogel had penetrated my rectal wall. I've been dealing with pain, pressure, rectal urgency & bleeding for over 2 months. The Dr. says that I should get some relief after the 90 day mark of the procedure. Has anyone else had to deal with this?”
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
7/21/23:
“Event Description:
It was reported to boston scientific corporation that a spaceoar vue device was implanted during a spaceoar vue implant procedure on (b)(6) 2023. Fiducial markers were placed transperineally prior to the hydrogel injection. The procedure was performed under general anesthesia. On (b)(6) 2023, was reported that the patient developed a fistula due to the hydrogel. The patient finished his external beam radiation treatment successfully. The patient was referred to an interventional radiologist for treatment. The fistula was reported as ongoing at the time of this report.”
“Event Description:
It was reported to boston scientific corporation that a spaceoar vue device was implanted during a spaceoar vue implant procedure on (b)(6) 2023. Fiducial markers were placed transperineally prior to the hydrogel injection. The procedure was performed under general anesthesia. On (b)(6) 2023, was reported that the patient developed a fistula due to the hydrogel. The patient finished his external beam radiation treatment successfully. The patient was referred to an interventional radiologist for treatment. The fistula was reported as ongoing at the time of this report.”
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
“It was reported to boston scientific corporation that a spaceoar vue device was implanted during a spaceoar vue implant procedure on an unknown date. Fiducials were place before the hydrogel injection. The patient was asymptomatic after the procedure and started his stereotactic body radiation therapy (sbrt). One month later the gastroenterologist said that the patient started having symptoms and that the patient had a new ulcer that had not been seen previously. The patient's physician thought the ulcer may be related to the spaceoar injection, since the stereotactic body radiation therapy (sbrt) plan was fine. The patient's gastroenterologist put him on mesalamine and supportive care. At time of this report the patient has been out from radiation treatment for about 2-3 months. It was suggested the patient will be in hyperbaric oxygen if his pain does not improve. The patient's physician reported later the patient was having "silicone-like output" in his bowel movements and severe painful spams. The hypothesis for this event was "there was an ulceration of the hydrogel through the mucosa causing this pain" therefore it was recommended to put the patient in stools softeners and anti-spasmodic to help with discomfort. No further information has been obtained despite good faith efforts.”
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Interesting:
Boston scientific corporation became aware of the following event through the article "seed lost to perineum from hydrogel spacer after brachytherapy for prostate cancer" written by makoto nakiri, md et al. According to the literature, the patient received hydrogel spacer injection, that was performed by transrectal ultrasound guidance, seven months after combined androgen blockade (cab) therapy initiated. Seventy seeds were placed during brachytherapy (bt) without complication or loss. The patient's external beam radiation therapy, prescribed dose 45 gy, was performed one month after bt. A pelvic magnetic resonance imaging (mri) was taken during normal post-planning, one month after hydrogel implantation, revealing no problems with the insertion. Six months later after bt and the hydrogel injection, the patient went to the hospital after the brachytherapy and complained of redness, pain, bleeding. Erythema was observed in addition to swelling and induration on the side of the perineal anus. A formation of the pinhole fistula in the center of the lesion was noted with serous effusion with loss of a seed from the fistula. Laboratory tests were performed, that revealed elevated c-reactive protein levels to 5. 91 mg/dl and elevated blood glucose levels to 230 mg/dl. In addition, the patient's hemoglobin a1c was 5. 8% before bt and had increased to 7. 6%. Abdominal computed tomography (ct) showed a high-density area suggestive of the seed on the right side of the perineum and inflammatory findings around the tissue. Pelvic magnetic resonance imaging showed a tunnel like discharge of hydrogel from the dorsal prostate to the perineum. The fistula was incised, the seed was removed, and drainage was performed. The perineal drainage and urine cultures performed were negative. The patient received antibiotic therapy and underwent wound cleaning. Thereafter, the inflammation improved based on receding erythema and reduced c-reactive protein levels. Indigo carmine was injected through the perineal fistula to evaluate for urethral and rectal fistulas, neither of which were observed. After the inflammation subsided, the fistula site was sutured. Spontaneous remission was observed following conservative treatment with antibiotics and drainage. Two years after treatment, no recurrence of prostate cancer or relapse of inflammation was noted. Retrospective imaging studies showed a seed placed near the coating on the right side of the dorsal prostatic margin had fallen out of the perineum. It was noted there were three factors thought to have contributed to this event, the first one was the injection of hydrogel could cause physical compression, resulting in ischemia changes around the perineum and rectum. The second factor discussed was the diabetes type 2 that the patient had. The last one was that the physician placed the seed along the outer capsule of the prostate. No further information has been obtained despite good faith efforts.
Boston scientific corporation became aware of the following event through the article "seed lost to perineum from hydrogel spacer after brachytherapy for prostate cancer" written by makoto nakiri, md et al. According to the literature, the patient received hydrogel spacer injection, that was performed by transrectal ultrasound guidance, seven months after combined androgen blockade (cab) therapy initiated. Seventy seeds were placed during brachytherapy (bt) without complication or loss. The patient's external beam radiation therapy, prescribed dose 45 gy, was performed one month after bt. A pelvic magnetic resonance imaging (mri) was taken during normal post-planning, one month after hydrogel implantation, revealing no problems with the insertion. Six months later after bt and the hydrogel injection, the patient went to the hospital after the brachytherapy and complained of redness, pain, bleeding. Erythema was observed in addition to swelling and induration on the side of the perineal anus. A formation of the pinhole fistula in the center of the lesion was noted with serous effusion with loss of a seed from the fistula. Laboratory tests were performed, that revealed elevated c-reactive protein levels to 5. 91 mg/dl and elevated blood glucose levels to 230 mg/dl. In addition, the patient's hemoglobin a1c was 5. 8% before bt and had increased to 7. 6%. Abdominal computed tomography (ct) showed a high-density area suggestive of the seed on the right side of the perineum and inflammatory findings around the tissue. Pelvic magnetic resonance imaging showed a tunnel like discharge of hydrogel from the dorsal prostate to the perineum. The fistula was incised, the seed was removed, and drainage was performed. The perineal drainage and urine cultures performed were negative. The patient received antibiotic therapy and underwent wound cleaning. Thereafter, the inflammation improved based on receding erythema and reduced c-reactive protein levels. Indigo carmine was injected through the perineal fistula to evaluate for urethral and rectal fistulas, neither of which were observed. After the inflammation subsided, the fistula site was sutured. Spontaneous remission was observed following conservative treatment with antibiotics and drainage. Two years after treatment, no recurrence of prostate cancer or relapse of inflammation was noted. Retrospective imaging studies showed a seed placed near the coating on the right side of the dorsal prostatic margin had fallen out of the perineum. It was noted there were three factors thought to have contributed to this event, the first one was the injection of hydrogel could cause physical compression, resulting in ischemia changes around the perineum and rectum. The second factor discussed was the diabetes type 2 that the patient had. The last one was that the physician placed the seed along the outer capsule of the prostate. No further information has been obtained despite good faith efforts.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Boston Scientific warns on some SpaceOAR systems

Boston Scientific warns on some SpaceOAR systems
Boston Scientific has issued an urgent field safety notice in Europe due to potential issues with its SpaceOAR systems.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Pelvic exenteration:
| Event Date 06/01/2023 |
| Event Type Injury |
| Event Description |
| It was reported to boston scientific corporation that a spaceoar device was implanted during a spaceoar implant procedure on an unknown date. It was reported a colorectal surgeon had to repair a fistula caused by spaceoar. It was also reported, at a later date, that the patient would be getting a pelvic exenteration. The patient's condition was reported as unknown. No further information has been obtained despite good faith efforts. |
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Embolism and left hemiparesis:
| Event Description |
| It was reported to boston scientific corporation that a spaceoar vue device was implanted during a spaceoar vue implant procedure on (b)(6) 2023. The scans of the placement showed that the hydrogel appears to be place into the peri-prostatic venous plexus. On (b)(6) 2023, presented with left side hemiparesis via ambulance and found to have an acute cerebrovascular accident in the right middle cerebral artery (mca). Therefore, the patient underwent emergency thrombectomy and an echocardiogram in hospital that was reported unremarkable. The patient recovered mostly back to the baseline strength and very minimal weakness on left side. The patient was reported as "fully recovered" at the time of this reported. No further information has been obtained despite good faith efforts. |
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
The majority of these reports are in patients being treated with SBRT and hypofractionation.
Looks ripe for litigation.
Looks ripe for litigation.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833

Rectourethral fistula following SpaceOAR gel placement for prostate cancer radiotherapy: A rare complication
After undergoing a SpaceOAR® gel placement prior to planned radiotherapy for Gleason 4 + 4 prostate cancer, a 70-year-old male experienced severe right buttock pain and urine passing from his rectum. A colonoscopy and follow-up ...
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
HBO to save the day

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov

The use of hyperbaric oxygen to treat actinic rectal fistula after SpaceOAR use and radiotherapy for prostate cancer: a case report - PubMed
Our report indicates that EBRT can lead to a severe rectum complication by causing inflammation for patients with a peri-SpaceOAR abscess. Furthermore, HBOT was effective for the peri-SpaceOAR abscess and rectal perforation associated with EBRT.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
These reports make me soooo nervous.
I still offer spaceOAR but certainly don't push it. I'd say about 30% of my prostates get it. It is very prevalent in my community, so patients are asking for it/about it.
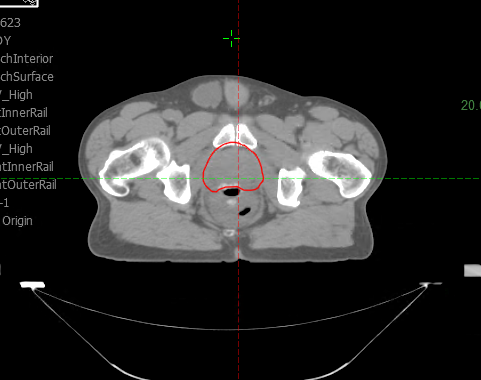
I know the VUE can be seen on CT but I think it's VERY important to get a post insertion MRI - it will show rectal wall infiltration much better. I don't offer spaceOAR to anyone that can't have an MRI.
I then carefully look at it and review with our prostate MRI folks. If any rectal wall infiltration they need to do a proctoscope and look at mucosa. If any mucosal alteration then you need to wait and not start radiation. I am convinced spaceOAR bad placement plus SBRT is a PROBLEM. If any concern at all about placement then I think they need switched to 28+ fractions.
I still offer spaceOAR but certainly don't push it. I'd say about 30% of my prostates get it. It is very prevalent in my community, so patients are asking for it/about it.
I know the VUE can be seen on CT but I think it's VERY important to get a post insertion MRI - it will show rectal wall infiltration much better. I don't offer spaceOAR to anyone that can't have an MRI.
I then carefully look at it and review with our prostate MRI folks. If any rectal wall infiltration they need to do a proctoscope and look at mucosa. If any mucosal alteration then you need to wait and not start radiation. I am convinced spaceOAR bad placement plus SBRT is a PROBLEM. If any concern at all about placement then I think they need switched to 28+ fractions.
What an absolute horrorshow. ALLLLLLL just to prevent a 1.5%-2% chance of telangiectatic (probably not a word but a helluva lot of fun to say out loud so I'm leaving it) bleeding that's easily taken care of with a CO2 laser*. Madness.
*Don't even get me started on the "it helps grade 2 toxicity" argument. Placement of the device itself leads to 100% chance of grade 2 GI toxicity.
*Don't even get me started on the "it helps grade 2 toxicity" argument. Placement of the device itself leads to 100% chance of grade 2 GI toxicity.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Here is a study that "suggests" due to the increased toxicities of hypofractionation that SPACEOAR/BARRIGEL should be utilized. I thought the toxicity of hypofractionation wasn't higher than conventional radiotherapy?

 jamanetwork.com
jamanetwork.com

Hyaluronic Acid Spacer for Hypofractionated Prostate Radiation Therapy
This randomized clinical trial examines whether a hyaluronic acid rectal spacer could improve rectal dosimetry and affect acute grade 2 or higher gastrointestinal toxic effects for hypofractionated radiation therapy.
Last edited:
D
deleted1111261
Thanks guys!
I just posted a collection of these from Maude on Twitter!
I just posted a collection of these from Maude on Twitter!
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
Thanks guys!
I just posted a collection of these from Maude on Twitter!
Prepare for silence or "I've never seen this in my clinic."
I have seen rectal wall infiltration in two cases, neither of whom I did their spaceOAR. I'm certainly not claiming I'm an expert on it. Probably a denominator at this point of ?50? . Fortunately they both have turned out fine.
I reached out to a lot of experts and got a lot of opinions. For anonymity I'll decline to say who I communicated with. Consensus was get a look at mucosa before doing anything. If mucosa intact and no symptoms and you really want to start then switch away from SBRT and do 28+. If mucosa issues then do not start treatment. Wait until it completely clears up and re-image before doing anything radiation wise.
Aside - at least in my training years ago the reps will tell you to "push through the rectal hump" to get in the space. I am confident many times the needle goes through mucosa then back out of mucosa and into the space. It's mostly fine, but when it's not fine it's a problem. A BIG problem.
D
deleted1111261
At the very least, adhere to study critieria?In what cases would you consider it justifiable.
Feels like there are believers and non believers. Not sure what decision rules you'd use as a non believer to justify it.
No T3, <80 cc volume, etc
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
I hate that not in my hands argument. This “device” needs to be able to translate into almost all clinics, otherwise it needs to be recalled.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
I hate that not in my hands argument. This “device” needs to be able to translate into almost all clinics, otherwise it needs to be recalled.
It's been a while since I've read the studies...
Did all of the patients on the randomized trials have post-spaceOAR MRI's?
Also I wonder what % of these MAUD cases are SBRT versus hypo or standard frac?
D
deleted1111261
The defenders are aggressive... Someone just replied "Do you know a similar liar for Barrigel? Thanks" Lol
- Joined
- Jun 1, 2011
- Messages
- 628
- Reaction score
- 869
They teach to go over the rectal hump these days.
- Joined
- Dec 27, 2019
- Messages
- 31
- Reaction score
- 59
Looks like there have also been at least 3 deaths resulting from MI immediately after placement. Seems that these were done with local. Very alarming.
- Joined
- Jul 26, 2007
- Messages
- 12,692
- Reaction score
- 2,311
My urologists are very old school and I've had (and continue to have) many discussions with them to bring them up to speed with what I'm trying to do for prostate cancer. For the most part progress has been made.
They had two really bad experiences with spaceOAR from the previous younger Radonc and have sworn off of it and hypofrac (they lump the two together - I've tried to discuss this but their opinion is set). Can't say I disagree with them on the spaceOAR front - I mean why risk it?
They had two really bad experiences with spaceOAR from the previous younger Radonc and have sworn off of it and hypofrac (they lump the two together - I've tried to discuss this but their opinion is set). Can't say I disagree with them on the spaceOAR front - I mean why risk it?
- Joined
- Jun 3, 2021
- Messages
- 20
- Reaction score
- 59
These reports make me soooo nervous.
I still offer spaceOAR but certainly don't push it. I'd say about 30% of my prostates get it. It is very prevalent in my community, so patients are asking for it/about it.
I know the VUE can be seen on CT but I think it's VERY important to get a post insertion MRI - it will show rectal wall infiltration much better. I don't offer spaceOAR to anyone that can't have an MRI.
I then carefully look at it and review with our prostate MRI folks. If any rectal wall infiltration they need to do a proctoscope and look at mucosa. If any mucosal alteration then you need to wait and not start radiation. I am convinced spaceOAR bad placement plus SBRT is a PROBLEM. If any concern at all about placement then I think they need switched to 28+ fractions.
Just say no - can reference this thread and see what they think after they are done reading.
- Joined
- Sep 20, 2004
- Messages
- 11,747
- Reaction score
- 11,839
These reports make me soooo nervous.
I still offer spaceOAR but certainly don't push it. I'd say about 30% of my prostates get it. It is very prevalent in my community, so patients are asking for it/about it.
I know the VUE can be seen on CT but I think it's VERY important to get a post insertion MRI - it will show rectal wall infiltration much better. I don't offer spaceOAR to anyone that can't have an MRI.
I then carefully look at it and review with our prostate MRI folks. If any rectal wall infiltration they need to do a proctoscope and look at mucosa. If any mucosal alteration then you need to wait and not start radiation. I am convinced spaceOAR bad placement plus SBRT is a PROBLEM. If any concern at all about placement then I think they need switched to 28+ fractions.
I've cited the maude data as well as my own experience regarding the one pt who required an elective colostomy for several months in the context of low proctitis rates in my practice pre hydrogel. Most pts usually good after thatJust say no - can reference this thread and see what they think after they are done reading.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
I will say the rate of rectal wall infiltration is significantly under-reported I bet.
After my scares I started looking really closely with a fellowship trained MRI pelvis radiologist (reads all our prostate and rectal protocol MRI's). He finds stuff way better than was found in the past.
if you don't look you're flying blind.
Of course many of these are clinically insignificant amounts of infiltration...but are you SURE it's clinically insignificant?
After my scares I started looking really closely with a fellowship trained MRI pelvis radiologist (reads all our prostate and rectal protocol MRI's). He finds stuff way better than was found in the past.
if you don't look you're flying blind.
Of course many of these are clinically insignificant amounts of infiltration...but are you SURE it's clinically insignificant?
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
prostate sim this week. Having pt come back to see if he has any rectal complaints and will probably get an mri
SBRT up to 40 Gy in 5 fx is perfectly safe without any gel whatsoever.
I always make sure patients understand that people are paid to place the device, and that payment is what is driving usage, which I very truly believe. The data show- unequivocally- that placement of the device results in 100% grade 2 toxicity and does not substantially reduce long-term grade 2 or 3 toxicity. The data via MAUDE have also shown several grade 5 toxicities. How many grade 5 toxicities are acceptable? I would argue the number is zero.
I always make sure patients understand that people are paid to place the device, and that payment is what is driving usage, which I very truly believe. The data show- unequivocally- that placement of the device results in 100% grade 2 toxicity and does not substantially reduce long-term grade 2 or 3 toxicity. The data via MAUDE have also shown several grade 5 toxicities. How many grade 5 toxicities are acceptable? I would argue the number is zero.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
It doesn’t pay that well.SBRT up to 40 Gy in 5 fx is perfectly safe without any gel whatsoever.
I always make sure patients understand that people are paid to place the device, and that payment is what is driving usage, which I very truly believe. The data show- unequivocally- that placement of the device results in 100% grade 2 toxicity and does not substantially reduce long-term grade 2 or 3 toxicity. The data via MAUDE have also shown several grade 5 toxicities. How many grade 5 toxicities are acceptable? I would argue the number is zero.
So I'm not sure it's the immediate financial bump from that actual procedure.
I think for early adopters it was a way to show a unique approach and a way to differentiate. Now they're committed to it. I do think it has helped side effects in the proton patients (have heard of clinics going from rectal balloon to no balloon needed with spaceOAR).
At least they did a randomized trial (though primary dosimetry endpoint is dumb).
Like a lot of other things in rad onc, I have a hard time being dogmatic about it. I'm just not sure it's worth it to reduce chance of a minor side effect for a slight increase in the risk of a MAJOR problem.
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
know of some radoncs that do a great job with the placement, very carefully under full sedation, but it is clearly not translating well into the community- have heard of disasters despite being placed by some excellent urologists.It doesn’t pay that well.
So I'm not sure it's the immediate financial bump from that actual procedure.
I think for early adopters it was a way to show a unique approach and a way to differentiate. Now they're committed to it. I do think it has helped side effects in the proton patients (have heard of clinics going from rectal balloon to no balloon needed with spaceOAR).
At least they did a randomized trial (though primary dosimetry endpoint is dumb).
Like a lot of other things in rad onc, I have a hard time being dogmatic about it. I'm just not sure it's worth it to reduce chance of a minor side effect for a slight increase in the risk of a MAJOR problem.
- Joined
- Mar 20, 2013
- Messages
- 1,912
- Reaction score
- 3,511
know of some radoncs that do a great job with the placement, very carefully under full sedation, but it is clearly not translating well into the community- have heard of disasters despite being placed by some excellent urologists.
That has been my experience.
When I place it it takes me forever. I am very careful and hyper paranoid. I'm certainly not an expert though. I really like it that the urologists place them, as I'm VERY busy right now and it helps my work flow a lot. So I haven't been placing them in some time now - if patient wants it then urology doing it.
But in speaking with reps and friends across the country - in general the rad oncs that do these are "more careful" than urlogists...with one exception - if you have a urologist doing transperineal biopsies, then they're really slick with that technique and spaceOARs go beautifully for them.
D
deleted1111261
I agree with transperineal bx / spacer being slick. Very different.
This is very not the same as the dude out here in rando MI that watches 10 cases and then just starts doing them.
This is very not the same as the dude out here in rando MI that watches 10 cases and then just starts doing them.
- Joined
- Nov 2, 2019
- Messages
- 3,497
- Reaction score
- 14,519
Look, Boston Scientific, Palette -
You guys had your chance to bribe me. I said it when I started this thread almost two years ago.
I hate the goo with the passion of a thousand burning suns. My OpenPayments record remains barren, though.
Message received.

You guys had your chance to bribe me. I said it when I started this thread almost two years ago.
I hate the goo with the passion of a thousand burning suns. My OpenPayments record remains barren, though.
Message received.
I think you hit the nail on the head. Prostate cancer treatment is boring, and it's tough to differentiate yourself by offering regular, standard-of-care treatment. Using SpaceOAR allows someone to differentiate themselves. The "benefit" to patients is secondary.I think for early adopters it was a way to show a unique approach and a way to differentiate. Now they're committed to it. I do think it has helped side effects in the proton patients (have heard of clinics going from rectal balloon to no balloon needed with spaceOAR).
- Joined
- Oct 4, 2017
- Messages
- 5,019
- Reaction score
- 9,790
yip, its their shtick.I think you hit the nail on the head. Prostate cancer treatment is boring, and it's tough to differentiate yourself by offering regular, standard-of-care treatment. Using SpaceOAR allows someone to differentiate themselves. The "benefit" to patients is secondary.
- Joined
- Sep 20, 2004
- Messages
- 11,747
- Reaction score
- 11,839
Sounds great in theory when your show them that models and pictures etc. No data needed!I think you hit the nail on the head. Prostate cancer treatment is boring, and it's tough to differentiate yourself by offering regular, standard-of-care treatment. Using SpaceOAR allows someone to differentiate themselves. The "benefit" to patients is secondary.
Similar threads
D
- Replies
- 100
- Views
- 5K
