It is no secret that I think it is pretty feasible to make a lot of money in psychiatry and that I don't lose sleep over midlevel encroachment. But that isn't to say I think everything about the field is good - the problems that bring me to the point of wanting to switch jobs or retire early are entirely different. I think the worst part of psychiatry is that you just have to eat a lot sh$t sometimes. Although actual lawsuits might be rare, the number of extremely stressful things that relate to patient experience, HR, risk management, provider engagement, threats of violence, threats of lawsuits, verbal abuse from patients, verbal abuse from families, and impossible situations in which there is no feasible path that balances the needs and preferences of the patient, system, caregivers and ones self is significant and feels almost persistent. Now that patients can read our records, I think this is just going to get worse. It seems like the biggest predictor of being able to tolerate these negative aspects of the role is an ability to not care that much. But I wonder if our field had just done a better job of defining the problems we can actually solve (far fewer than most people think), and the tools/training we need (broad and extensive), we wouldn't be in a position where people think that prescribing enough prozac will prevent mass shootings, or that behavioral health treatment is an antidote for broad societal dysfunctions. The status quo is one of overpromising and under-delivering and it is therefore unsurprising that many people are dissatisfied with their experience on both sides of the table. It is wearing.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Moral Injury and Burnout
- Thread starter SmallBird
- Start date
hippopotamusoath
Full Member
- Joined
- Nov 13, 2022
- Messages
- 49
- Reaction score
- 106
I think about this idea a lot. I alluded to some of this in a previous post, but the situation is dire--there are very few of us, and we're staring down an increasingly severe psychiatrist deficit. Out of total number of psychiatrists, something like 40 or 50% take cash-only, obviously providing services to a very specific type of patient population. Then, as a field, we have become grabby--we have taken on a lot of problems as psychiatric that are social, and which we have very little chance of solving with the interventions available to us.
I think our field is going to become increasingly irrelevant if we don't make some fundamental changes. We are moving towards psychiatry becoming an interesting footnote in medicine--a dwindling number of people practicing an esoteric art for the worried well, and a few others who make valiant attempts at treating poverty with long-acting injectables. In my opinion, our current trajectory does not represent a serious approach to solving our field's problems.
I think we need to collectively make a decision--either we restrict our input to the things we can reasonably intervene on, or we insist on moving into public policy, advocacy, and other types of public health leadership which could reasonably improve many of the "psychiatric problems" we are boxed into treating with medications.
I'd be fine being held accountable for the problem of suicide if you gave me substantial power into crafting safe gun storage laws, red flag laws, etc. I'm not fine being held accountable in order to salve society's anxiety about the fact that suicide is inherently individual, multi-factorial, and the complex final endpoint of about a dozen systemic failures, most of which I have exactly zero ability to influence.
I respect our colleagues who have gone into cash private practices. It might not be doing the greatest good for the greatest number, but it is providing a valuable service to the individuals who can access it, and it seems to be a healthy situation for the physicians involved. They have opted out of the corrupt insurance system, and the more people who do that, the more likely that enterprise is to be forced into reform.
My personal path forward is to spend my early career seeing a lot of patients, and then slowly reducing my patient contact and increasing my time on leadership and policy in an attempt to make mental health efforts in my region more rational. If all else fails, I will start a cash private practice, and accept that I can't fundamentally change our broken system, but I can refuse to engage with the corrupt insurance system while I do a little good for my small panel of patients.
I think our field is going to become increasingly irrelevant if we don't make some fundamental changes. We are moving towards psychiatry becoming an interesting footnote in medicine--a dwindling number of people practicing an esoteric art for the worried well, and a few others who make valiant attempts at treating poverty with long-acting injectables. In my opinion, our current trajectory does not represent a serious approach to solving our field's problems.
I think we need to collectively make a decision--either we restrict our input to the things we can reasonably intervene on, or we insist on moving into public policy, advocacy, and other types of public health leadership which could reasonably improve many of the "psychiatric problems" we are boxed into treating with medications.
I'd be fine being held accountable for the problem of suicide if you gave me substantial power into crafting safe gun storage laws, red flag laws, etc. I'm not fine being held accountable in order to salve society's anxiety about the fact that suicide is inherently individual, multi-factorial, and the complex final endpoint of about a dozen systemic failures, most of which I have exactly zero ability to influence.
I respect our colleagues who have gone into cash private practices. It might not be doing the greatest good for the greatest number, but it is providing a valuable service to the individuals who can access it, and it seems to be a healthy situation for the physicians involved. They have opted out of the corrupt insurance system, and the more people who do that, the more likely that enterprise is to be forced into reform.
My personal path forward is to spend my early career seeing a lot of patients, and then slowly reducing my patient contact and increasing my time on leadership and policy in an attempt to make mental health efforts in my region more rational. If all else fails, I will start a cash private practice, and accept that I can't fundamentally change our broken system, but I can refuse to engage with the corrupt insurance system while I do a little good for my small panel of patients.
Last edited:
- Joined
- Feb 15, 2009
- Messages
- 18,060
- Reaction score
- 23,840
While I agree and I also plan to retire as soon as I can due to most of these things, patients have been able to read their charts in the VA for a long time now. That particular ability hasn't changed anything for me and hasn't been nearly as much of a hassle as I had thought, fortunately. Sometimes a patient demands I remove a statement that reported some unflattering behavior. I just say "no, those are the facts" and that's been the end of it. That patient then has to decide whether to work with me on their problems, or they go find another psychiatrist, which suits me either way.
Yeah, my patients have always been provided a copy of their records form me, both within and outside of the VA. Never been a problem, especially as I go through everything that is in the report verbally with them at a feedback session. Also, under the vast majority of circumstances, patients have always had access to their records if requested. No idea why patients being more easily being able to see their records is this terrible thing.
- Joined
- Nov 6, 2009
- Messages
- 427
- Reaction score
- 568
Really appreciate this thread right now. Every time someone mentions "mental health" after another mass shooting or another horrific event I fall ever so slightly more into despair. The gap between what people (patients, families, policy makers, the media) thinks we can do and what we can actually do just grows wider every day.
I've been wondering about how telehealth is playing into this as well. It's definitely a good for some patients in increasing access, but in my setting we're also noticing a lot more abuse and harassment by patients via MyChart, angry phone conversations, etc that are outstripping what we saw pre-pandemic. I wonder if there's something about being able to scream into a phone or through a keyboard that lets patients and families see us even more as pill machines rather than people, and to be treated like you would treat a sever who screwed up your dinner order.
I work in a public CMHC setting with an academic bent, and there are certain subspecialty teams here that I work on that provide exceptional care, I would argue the best in the area even over and above some of the big name places. The amount of abuse we've been seeing from our patients recently has just been so demoralizing for our staff. Some of it is almost comical when you think about it (accusing me or a therapist colleague of being in it for the money when we're all salaried at a predominantly Medicaid clinic lol), but we're all just tired.
I have a moral commitment to this kind of work and can't imagine ever leaving full time for private practice, but it's so taxing.
There was a great op-ed in the Times yesterday that hit on some of the themes of this thread, would definitely recommend a read: Opinion | Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System.
I've been wondering about how telehealth is playing into this as well. It's definitely a good for some patients in increasing access, but in my setting we're also noticing a lot more abuse and harassment by patients via MyChart, angry phone conversations, etc that are outstripping what we saw pre-pandemic. I wonder if there's something about being able to scream into a phone or through a keyboard that lets patients and families see us even more as pill machines rather than people, and to be treated like you would treat a sever who screwed up your dinner order.
I work in a public CMHC setting with an academic bent, and there are certain subspecialty teams here that I work on that provide exceptional care, I would argue the best in the area even over and above some of the big name places. The amount of abuse we've been seeing from our patients recently has just been so demoralizing for our staff. Some of it is almost comical when you think about it (accusing me or a therapist colleague of being in it for the money when we're all salaried at a predominantly Medicaid clinic lol), but we're all just tired.
I have a moral commitment to this kind of work and can't imagine ever leaving full time for private practice, but it's so taxing.
There was a great op-ed in the Times yesterday that hit on some of the themes of this thread, would definitely recommend a read: Opinion | Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System.
When patients with personality disorders are hospitalized there is a need to document certain interactions in detail to ensure that the nuances of their clinical presentation can be appreciated by subsequent providers and to justify complex care decisions. There are circumstances under which patients who exhibit treatment interfering behaviors or have histrionic or narcissistic tendencies may use this material to monopolize the clinical interviews during their inpatient stays at the expense of being able to spend enough time discussing care plans or providing therapeutic input. It is already challenging when patients want to spend a lot of time complaining about what was said to them by a nurse, or a perceived mistake in their med rec - this just creates a huge amount of additional fodder for a process that is typically not therapeutic.Yeah, my patients have always been provided a copy of their records form me, both within and outside of the VA. Never been a problem, especially as I go through everything that is in the report verbally with them at a feedback session. Also, under the vast majority of circumstances, patients have always had access to their records if requested. No idea why patients being more easily being able to see their records is this terrible thing.
Really appreciate this thread right now. Every time someone mentions "mental health" after another mass shooting or another horrific event I fall ever so slightly more into despair. The gap between what people (patients, families, policy makers, the media) thinks we can do and what we can actually do just grows wider every day.
I've been wondering about how telehealth is playing into this as well. It's definitely a good for some patients in increasing access, but in my setting we're also noticing a lot more abuse and harassment by patients via MyChart, angry phone conversations, etc that are outstripping what we saw pre-pandemic. I wonder if there's something about being able to scream into a phone or through a keyboard that lets patients and families see us even more as pill machines rather than people, and to be treated like you would treat a sever who screwed up your dinner order.
I work in a public CMHC setting with an academic bent, and there are certain subspecialty teams here that I work on that provide exceptional care, I would argue the best in the area even over and above some of the big name places. The amount of abuse we've been seeing from our patients recently has just been so demoralizing for our staff. Some of it is almost comical when you think about it (accusing me or a therapist colleague of being in it for the money when we're all salaried at a predominantly Medicaid clinic lol), but we're all just tired.
I have a moral commitment to this kind of work and can't imagine ever leaving full time for private practice, but it's so taxing.
There was a great op-ed in the Times yesterday that hit on some of the themes of this thread, would definitely recommend a read: Opinion | Doctors Aren’t Burned Out From Overwork. We’re Demoralized by Our Health System.
Thank you for your commitment to what you do. It is somewhat better being in a setting where you have access to more tools than just medication, which it sounds like is the case at your CMHC.
I think part of what makes this more difficult is that the misalignment is not only coming from patients, families, and political influences, but even leaders in our field. I couldn't believe it but the Lancet just published a clinical trial that reported only on the feasibility and acceptability of a new M4 cholinergic modulator for psychosis. That a new, probably minimally helpful medication is being viewed as the most important new science in our field suggest that academics are truly disconnected from the barriers we are facing in being successful at improving lives and reducing suicide. By contrast we don't hear about which efforts to keep psychotic people from having to come to the hospital are proving to be most effective across the country.
- Joined
- Sep 12, 2010
- Messages
- 6,101
- Reaction score
- 3,090
Exactly.When patients with personality disorders are hospitalized there is a need to document certain interactions in detail to ensure that the nuances of their clinical presentation can be appreciated by subsequent providers and to justify complex care decisions. There are circumstances under which patients who exhibit treatment interfering behaviors or have histrionic or narcissistic tendencies may use this material to monopolize the clinical interviews during their inpatient stays at the expense of being able to spend enough time discussing care plans or providing therapeutic input. It is already challenging when patients want to spend a lot of time complaining about what was said to them by a nurse, or a perceived mistake in their med rec - this just creates a huge amount of additional fodder for a process that is typically not therapeutic.
- Joined
- Feb 15, 2009
- Messages
- 18,060
- Reaction score
- 23,840
When patients with personality disorders are hospitalized there is a need to document certain interactions in detail to ensure that the nuances of their clinical presentation can be appreciated by subsequent providers and to justify complex care decisions. There are circumstances under which patients who exhibit treatment interfering behaviors or have histrionic or narcissistic tendencies may use this material to monopolize the clinical interviews during their inpatient stays at the expense of being able to spend enough time discussing care plans or providing therapeutic input. It is already challenging when patients want to spend a lot of time complaining about what was said to them by a nurse, or a perceived mistake in their med rec - this just creates a huge amount of additional fodder for a process that is typically not therapeutic.
And, for certain circumstances, there still exists a mechanism to block the notes, at least temporarily, if they meet the criteria of exceptions within the law. These are very similar to the exceptions that existed before with regards to patients requesting notes. I've worked on many inpatient units, in neuropsych, intensive inpatient PTSD and SUD treatment (and lots of comorbid Axis II). Never personally had a problem, and the problem was never raised in multidisciplinary team meetings. I really do not think it is that challenging to **** this down in the largely occasional circumstance that a patient brings up a chart comment.
- Joined
- Oct 13, 2008
- Messages
- 4,154
- Reaction score
- 7,957
Thank you for your commitment to what you do. It is somewhat better being in a setting where you have access to more tools than just medication, which it sounds like is the case at your CMHC.
I think part of what makes this more difficult is that the misalignment is not only coming from patients, families, and political influences, but even leaders in our field. I couldn't believe it but the Lancet just published a clinical trial that reported only on the feasibility and acceptability of a new M4 cholinergic modulator for psychosis. That a new, probably minimally helpful medication is being viewed as the most important new science in our field suggest that academics are truly disconnected from the barriers we are facing in being successful at improving lives and reducing suicide. By contrast we don't hear about which efforts to keep psychotic people from having to come to the hospital are proving to be most effective across the country.
I mean, that research is out there, just in lower IF factor/prestige journals. Journal of Psychiatric Services is fairly solid. Not all of the papers you find there are created equal by any means, but I respect the hell out of the editor and have definitely read about some very interesting systems/delivery-of-care type innovations in it in the past.
hippopotamusoath
Full Member
- Joined
- Nov 13, 2022
- Messages
- 49
- Reaction score
- 106
I think our insistence on pouring our resources into "biological psychiatry" has been a colossal failure, and has historical roots that are probably well-known to most on this forum. So here we go--another mediocre medicine to fatten the pockets of a drug company, and cause maybe some slight benefit to a few patients.Thank you for your commitment to what you do. It is somewhat better being in a setting where you have access to more tools than just medication, which it sounds like is the case at your CMHC.
I think part of what makes this more difficult is that the misalignment is not only coming from patients, families, and political influences, but even leaders in our field. I couldn't believe it but the Lancet just published a clinical trial that reported only on the feasibility and acceptability of a new M4 cholinergic modulator for psychosis. That a new, probably minimally helpful medication is being viewed as the most important new science in our field suggest that academics are truly disconnected from the barriers we are facing in being successful at improving lives and reducing suicide. By contrast we don't hear about which efforts to keep psychotic people from having to come to the hospital are proving to be most effective across the country.
Why aren't we insisting to our leadership that we pour money and research resources into psychosocial interventions at the same rate? Why don't we have a free, nationally-available computerized CBT program for anxiety, so every anxious patient has at least one quality intervention available with just an internet connection? Why haven't we dumped money into the community mental health system? Why haven't we brought back asylums for the most severely ill patients? Why haven't we built a system of unlocked crisis centers as an alternative to unhelpful emergency department visits for our BPD patients in crisis?
The public cries for "access to mental health," but I don't think they realize how disappointing that access will be, if they ever get it...
- Joined
- Nov 6, 2009
- Messages
- 427
- Reaction score
- 568
I would like to quote every post in this thread and send it to the heads of NIMH and SAMSHA.
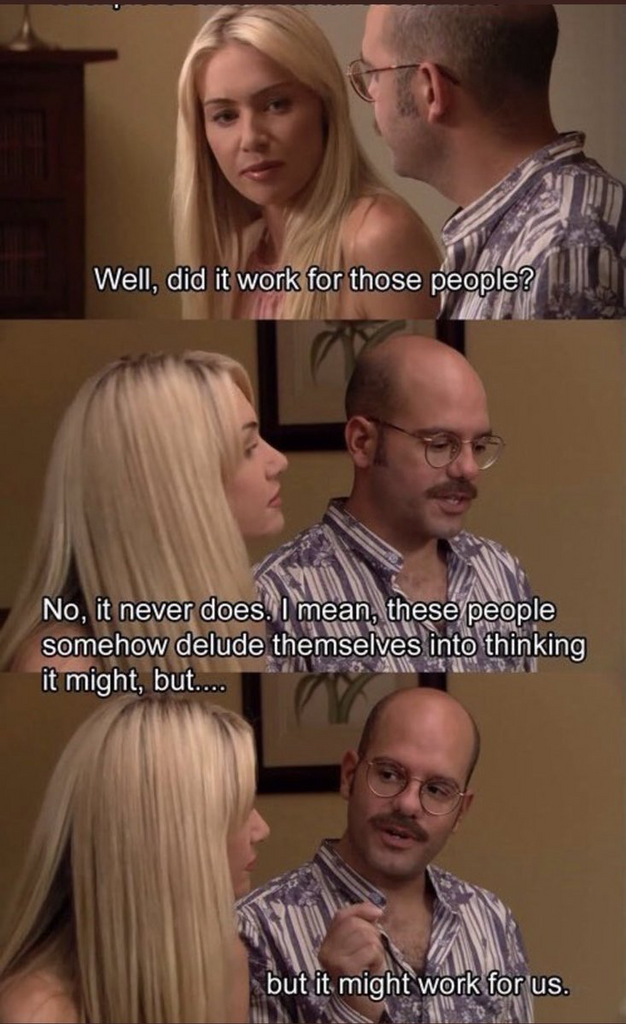
Every time a new antipsychotic comes on the market promising this time will be the first time we've had a real advance since clozapine:
Another plug for Psych Services, really wonderful journal and Lisa Dixon (the editor) is someone who cares deeply about finding and disseminating health systems interventions to help people access the treatments we have that work but are basically unavailable to 99% of the population.
Thank you for your commitment to what you do. It is somewhat better being in a setting where you have access to more tools than just medication, which it sounds like is the case at your CMHC.
I think part of what makes this more difficult is that the misalignment is not only coming from patients, families, and political influences, but even leaders in our field. I couldn't believe it but the Lancet just published a clinical trial that reported only on the feasibility and acceptability of a new M4 cholinergic modulator for psychosis. That a new, probably minimally helpful medication is being viewed as the most important new science in our field suggest that academics are truly disconnected from the barriers we are facing in being successful at improving lives and reducing suicide. By contrast we don't hear about which efforts to keep psychotic people from having to come to the hospital are proving to be most effective across the country.
Every time a new antipsychotic comes on the market promising this time will be the first time we've had a real advance since clozapine:
I mean, that research is out there, just in lower IF factor/prestige journals. Journal of Psychiatric Services is fairly solid. Not all of the papers you find there are created equal by any means, but I respect the hell out of the editor and have definitely read about some very interesting systems/delivery-of-care type innovations in it in the past.
Another plug for Psych Services, really wonderful journal and Lisa Dixon (the editor) is someone who cares deeply about finding and disseminating health systems interventions to help people access the treatments we have that work but are basically unavailable to 99% of the population.
It's really stunning to realize that we actually know what works for many people with many conditions. Doesn't mean that there isn't room to improve existing treatments or that some people fail to respond even to gold standard interventions (ex. treatment resistant schizophrenia with no response to clozapine or ECT, really refractory personality disorders) of course. But the difference between the amount of money we would spend helping people access existing effective interventions (supported employment in psychosis, peer support for SUD, bog standard CBT for panic disorder) vs the billions we pour into drug research to maybe someday find a drug that's 5% more effective than risperidone makes me want to become the joker.I think our insistence on pouring our resources into "biological psychiatry" has been a colossal failure, and has historical roots that are probably well-known to most on this forum. So here we go--another mediocre medicine to fatten the pockets of a drug company, and cause maybe some slight benefit to a few patients.
Why aren't we insisting to our leadership that we pour money and research resources into psychosocial interventions at the same rate? Why don't we have a free, nationally-available computerized CBT program for anxiety, so every anxious patient has at least one quality intervention available with just an internet connection? Why haven't we dumped money into the community mental health system? Why haven't we brought back asylums for the most severely ill patients? Why haven't we built a system of unlocked crisis centers as an alternative to unhelpful emergency department visits for our BPD patients in crisis?
The public cries for "access to mental health," but I don't think they realize how disappointing that access will be, if they ever get it...
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
But I wonder if our field had just done a better job of defining the problems we can actually solve (far fewer than most people think), and the tools/training we need (broad and extensive), we wouldn't be in a position where people think that prescribing enough prozac will prevent mass shootings, or that behavioral health treatment is an antidote for broad societal dysfunctions. The status quo is one of overpromising and under-delivering and it is therefore unsurprising that many people are dissatisfied with their experience on both sides of the table. It is wearing.
There are jobs that involve designing and implementing novel policy interventions, and if you want to get there from MD-psychiatry you could get there by doing a policy fellowship (which is not competitive at all), then get a job in a public policy leadership role, etc. etc.
There are plenty of grants that are stipulated in this area, but the way in which you would get them is long and tedious.
This path generally doesn't pay well, and there is a big component w.r.t. advocacy, political work, etc.
So, you could complain about it, or you can walk the walk and actually do what you think would help, but generally when I bring this up to actual practicing psychiatrists, they have no interest in cutting their salary 30% and filing 100-page federal and state grant applications. So this is all just useless whining.
I think our insistence on pouring our resources into "biological psychiatry" has been a colossal failure, and has historical roots that are probably well-known to most on this forum. So here we go--another mediocre medicine to fatten the pockets of a drug company, and cause maybe some slight benefit to a few patients.
Why aren't we insisting to our leadership that we pour money and research resources into psychosocial interventions at the same rate? Why don't we have a free, nationally-available computerized CBT program for anxiety, so every anxious patient has at least one quality intervention available with just an internet connection? Why haven't we dumped money into the community mental health system? Why haven't we brought back asylums for the most severely ill patients? Why haven't we built a system of unlocked crisis centers as an alternative to unhelpful emergency department visits for our BPD patients in crisis?
The public cries for "access to mental health," but I don't think they realize how disappointing that access will be, if they ever get it...
Disagree. The reason that psychiatry pivoted to biological is that psychosocial interventions had been "trialed" for many hundreds of years. In fact, you can plausibly argue that psychosocial interventions are not scientific. Luminaries in the field are trying to make it more scientific, so to speak, but this is not a clean process at all. The only intervention that reliably reduces psychosis is antipsychotic medications/ECT, and you know how effective they are on average. In specific, incidental cases, they can be life-changing.
Psychosocial interventions are low prestige and low effect size. This is generally true throughout all medicine. You can say okay CBT works better than antidepressant meds for X. Sure. But really what it says is that CBT is equally INEFFECTIVE as meds are for X. Compared to large effect size interventions (i.e. clozapine, ECT, addiction meds, ADHD meds), therapy is at best adjunctive, and often do nothing (several large trials show this type of results).
If we had no meds and other somatic treatments, you'd get paid less, the residency programs won't be that competitive. Cash practices won't be nearly as widespread (demand won't be there), and the practice would be much more usurped by "mid-levels". So you can't really complain about both (low-prestige/mid-level penetrance and lack of access/indigent patients being aggressive) at the same time. If you want to be high prestige you need to be scientific, technical, exclusive (small number of physicians capable of delivery), and (hopefully) large effect size. I can't think of a single high-prestige effort in medicine that isn't like this.
I think psychiatry needs to split more (and this is indeed the tendency here in the real world). More "procedural"/"medical"/"specialized" subspecialties (child/addiction/"interventional", etc.) will be much more focused. Training on TMS, stellate ganglion, ketamine, other psychedelics, other somatics (obesity meds, hormone) will become more widespread. Psychotherapy-focused specialists would have their own subspecialty for "cosmetic/existential psychiatry", as most analytic institutes shut down and only the highest prestige ones remain and only take a handful of MDs a year. General psychiatry/public health-focused portions will include more management/business school curricula on training "mid-levels" on the delivery and budgeting of psychosocial interventions effectively. These pathways will become more formalized, even though as is they kind of already are (i.e. people who want to practice "cosmetic" need to match into a handful of programs that have analytic institutes, a wealthy patient base, etc). The future of psychiatry is that if it really wants to be "the new derm" it needs to act more like it.
Last edited:
If I think of every difficult situation I've dealt with in the last few years of high volume inpatient adult and pediatric work, I think maybe 5% of the time the issue was that I wished I had a different or better medication.
With psychotic patients, unless there is a plausible biological intervention to help restore lost cognitive function from chronic illness, what I need is not another medication but a place they can sleep that doesn't kick them out when they act a bit different, where people are reasonably nice, and where they don't have to file taxes or pay bills. This would help the vast majority of patients that have been challenges. For patients with mood and anxiety disorders, it is bizarrely difficult to find therapists trained in behavioral activation and exposures.
A challenge on a broader level is that when patients come to the ERs from families, nursing homes, group homes, or accompanied by their personality disorders, our ability to follow-through on an assessment that the core issue is not one which will benefit from psychiatric hospitalization is often absent. These individuals do have tremendous needs and because they cannot be met elsewhere the default is that we have to work with them despite it being ineffective. We need both an investment in diversion options as well as a best practice framework that supports not admitting in these cases. But probably if you don't admit a demented person for the 10th time and you are sued the expert witness will be someone who did the ridiculous IV alzaheimers drug trials and will say it was your fault for not upping their donepezil.
With psychotic patients, unless there is a plausible biological intervention to help restore lost cognitive function from chronic illness, what I need is not another medication but a place they can sleep that doesn't kick them out when they act a bit different, where people are reasonably nice, and where they don't have to file taxes or pay bills. This would help the vast majority of patients that have been challenges. For patients with mood and anxiety disorders, it is bizarrely difficult to find therapists trained in behavioral activation and exposures.
A challenge on a broader level is that when patients come to the ERs from families, nursing homes, group homes, or accompanied by their personality disorders, our ability to follow-through on an assessment that the core issue is not one which will benefit from psychiatric hospitalization is often absent. These individuals do have tremendous needs and because they cannot be met elsewhere the default is that we have to work with them despite it being ineffective. We need both an investment in diversion options as well as a best practice framework that supports not admitting in these cases. But probably if you don't admit a demented person for the 10th time and you are sued the expert witness will be someone who did the ridiculous IV alzaheimers drug trials and will say it was your fault for not upping their donepezil.
I do plenty. There is a spectrum between useless whining and reorienting your entire career. Developing ideas with thoughtful colleagues online is a productive option.There are jobs that involve designing and implementing novel policy interventions, and if you want to get there from MD-psychiatry you could get there by doing a policy fellowship (which is not competitive at all), then get a job in a public policy leadership role, etc. etc.
There are plenty of grants that are stipulated in this area, but the way in which you would get them is long and tedious.
This path generally doesn't pay well, and there is a big component w.r.t. advocacy, political work, etc.
So, you could complain about it, or you can walk the walk and actually do what you think would help, but generally when I bring this up to actual practicing psychiatrists, they have no interest in cutting their salary 30% and filing 100-page federal and state grant applications. So this is all just useless whining.
- Joined
- Nov 6, 2009
- Messages
- 427
- Reaction score
- 568
I am a health services researcher doing this. I also do not think it is whining for practicing clinicians to note how broken the system is and wish things were different while primarily seeing patients.There are jobs that involve designing and implementing novel policy interventions, and if you want to get there from MD-psychiatry you could get there by doing a policy fellowship (which is not competitive at all), then get a job in a public policy leadership role, etc. etc.
There are plenty of grants that are stipulated in this area, but the way in which you would get them is long and tedious.
This path generally doesn't pay well, and there is a big component w.r.t. advocacy, political work, etc.
So, you could complain about it, or you can walk the walk and actually do what you think would help, but generally when I bring this up to actual practicing psychiatrists, they have no interest in cutting their salary 30% and filing 100-page federal and state grant applications. So this is all just useless whining.
CBT for psychosis? Effect size is small/moderate but comparable to drugs we use all the time (ex. SRIs). This is not a replacement for antipsychotic medication therapy but this above claim is not supported by the evidence.Disagree. The reason that psychiatry pivoted to biological is that psychosocial interventions had been "trialed" for many hundreds of years. In fact, you can plausibly argue that psychosocial interventions are not scientific. The only intervention that reliably reduces psychosis is antipsychotic medications/ECT, and you know how effective they are on average. In specific, incidental cases, they can be life-changing.
Psychosocial interventions are low prestige and low effect size. This is generally true throughout all medicine.
To say nothing of peer support, supported employment, family psychoeducation, and other evidence based practices found to reduce psychosis relapse in the RAISE trial as well as in other meta-analyses: Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis
And of course this is even more true outside of psychosis where psychotherapies have equal or greater effect sizes than medications.
I'm frankly befuddled by this post.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
I am a health services researcher doing this. I also do not think it is whining for practicing clinicians to note how broken the system is and wish things were different while primarily seeing patients.
I mean... Isn't it though? What use is it? Why should I waste my time listening to you whine about "the system" all day when I can use the same time to write another grant to actually do something about "the system"? Maybe I can get PAID to listen to you whine in a focus group instead--or be your THERAPIST and actually HELP you.
CBT for psychosis? Effect size is small/moderate but comparable to drugs we use all the time (ex. SRIs). This is not a replacement for antipsychotic medication therapy but this above claim is not supported by the evidence.
Why isn't it a replacement? I think you are making my argument for me here.
To say nothing of peer support, supported employment, family psychoeducation, and other evidence based practices found to reduce psychosis relapse in the RAISE trial as well as in other meta-analyses: Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis
Sure, psychosocial interventions work. I'm not disputing that at all. What I am saying is that psychosocial interventions will ALWAYS be low prestige. UNLESS they are themselves ULTRASPECIALIZED (psychoanalysis).
There are high-prestige CBT for psychosis practices, but they are extremely rare because there's no demand. If you create a fellowship for psychosis and get all kinds of certifications for exclusivity, you might be able to advocate for the institutions to pay more for that. As is, my question is why not pay an SW to deliver this to people who have psychosis? Of course there's no good reason not to do that. This means your job as the MD is really to become the MBA to manage a horde of SWs to quality assure that they are actually providing CBT for psychosis, which was exactly my point originally.
We are talking in parallel. Things that work are not prestigious and won't get paid. Diet and exercise work really well. Maybe you should get paid more as a dietician or personal trainer. Maybe Medicaid should pay $1000 a month for people to exercise. Good luck getting that passed in Congress. This is true throughout medicine. Do you want the specialty to be prestigious and well-paid, or do you want to universalize things that get paid by the government? You can't get both. So you should just split the specialty into two and let people pursue what they want for their career--which is exactly what is already happening.And of course this is even more true outside of psychosis where psychotherapies have equal or greater effect sizes than medications.
I'm frankly befuddled by this post.
Last edited:
I guess I can see an argument for not making psychosocial interventions the core of our field. But they are what the vast majority of our patients need. The problem is the misalignment. I don't really see much chance of a parallel mechanism for supporting individuals with mental illnesses being created so I think we are stuck with this gigantic mission and so I think the best focus should be on making sure it doesn't get even bigger (lets draw the line at mass shootings) and that we have the tools to address it (which are psychosocial in a large proportion of cases).Disagree. The reason that psychiatry pivoted to biological is that psychosocial interventions had been "trialed" for many hundreds of years. In fact, you can plausibly argue that psychosocial interventions are not scientific. Luminaries in the field are trying to make it more scientific, so to speak, but this is not a clean process at all. The only intervention that reliably reduces psychosis is antipsychotic medications/ECT, and you know how effective they are on average. In specific, incidental cases, they can be life-changing.
Psychosocial interventions are low prestige and low effect size. This is generally true throughout all medicine. You can say okay CBT works better than antidepressant meds for X. Sure. But really what it says is that CBT is equally INEFFECTIVE as meds are for X. Compared to large effect size interventions (i.e. clozapine, ECT, addiction meds, ADHD meds), therapy is at best adjunctive, and often do nothing (several large trials show this type of results).
If we had no meds and other somatic treatments, you'd get paid less, the residency programs won't be that competitive. Cash practices won't be nearly as widespread (demand won't be there), and the practice would be much more usurped by "mid-levels". So you can't really complain about both (low-prestige/mid-level penetrance and lack of access/indigent patients being aggressive) at the same time. If you want to be high prestige you need to be scientific, technical, exclusive (small number of physicians capable of delivery), and (hopefully) large effect size. I can't think of a single high-prestige effort in medicine that isn't like this.
I think psychiatry needs to split more (and this is indeed the tendency here in the real world). More "procedural"/"medical"/"specialized" subspecialties (child/addiction/"interventional", etc.) will be much more focused. Training on TMS, stellate ganglion, ketamine, other psychedelics, other somatics (obesity meds, hormone) will become more widespread. Psychotherapy-focused specialists would have their own subspecialty for "cosmetic/existential psychiatry", as most analytic institutes shut down and only the highest prestige ones remain and only take a handful of MDs a year. General psychiatry/public health-focused portions will include more management/business school curricula on training "mid-levels" on the delivery and budgeting of psychosocial interventions effectively. These pathways will become more formalized, even though as is they kind of already are (i.e. people who want to practice "cosmetic" need to match into a handful of programs that have analytic institutes, a wealthy patient base, etc). The future of psychiatry is that if it really wants to be "the new derm" it needs to act more like it.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
Sure. You *could* address it in a small number of patients in private practice, and over a number of years make a huge impact in a small number of patients. But then you tell yourself this isn't "morally good" because rich people apparently don't deserve good mental health and torture yourself until you retire. LOL. I don't know what to tell you here.I guess I can see an argument for not making psychosocial interventions the core of our field. But they are what the vast majority of our patients need. The problem is the misalignment. I don't really see much chance of a parallel mechanism for supporting individuals with mental illnesses being created so I think we are stuck with this gigantic mission and so I think the best focus should be on making sure it doesn't get even bigger (lets draw the line at mass shootings) and that we have the tools to address it (which are psychosocial in a large proportion of cases).
- Joined
- Mar 24, 2014
- Messages
- 5,528
- Reaction score
- 6,556
I don’t know if I agree that the psychosocial interventions always have to be low prestige. I think that dynamic is part of the problem with mental health treatment.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
It's not always low prestige. Prestige is associated with exclusivity, expensiveness, and the demand of people who can pay. It's not associated with necessity.I don’t know if I agree that the psychosocial interventions always have to be low prestige. I think that dynamic is part of the problem with mental health treatment.
Plenty of psychotherapists (and not just MDs) have exclusive, expensive, and high-demand practices. They just don't address issues relating to people who can't afford their services.
There is NOT a single service that aims towards public welfare and the indigent that's considered high prestige, not now, not in history, not in any other culture. That's literally the definition of prestige. People need to clarify their thoughts. People equate virtue with prestige. Many jobs relating to public welfare are *necessary* and *virtuous*, and *valuable*, but they aren't "prestigious". There are jobs that very obviously are both virtuous and prestigious, many are in medicine (transplant surgery, etc). High-end practices in psychiatry that are very specialized in technical expertise (i.e. pediatric psychopharmacologists) likely fall into this category, but the judgment call here is not nearly as obvious. Similar things exist in psychotherapy (specialized psychotherapists for say, athletes). This dynamic is not limited to mental health. This is a feature of the entire "capitalist" system. So you say okay I would rather reform the system at large so that I make sure that people who specialized high demand services cap their fees so that poor people who also need it can get access to it. This basically is what happened in communist countries. It doesn't work. Brute force centralized organization of supply and demand never works.
This is not to say that the current mental health system is perfect. Not at all. My point is that the systems-level issues are very specific and detail driven, and when you talk in personal, emotional, and philosophical terms, you suppress actual productive discussion of actual problems that are treatable via policy interventions. And you need to have a more definable clarity in thinking: do you really care about "the system" or do you just want to get a new job? In general, I find that people who complain about "the system" really just want a new job but use "the system" as a post hoc justification for making concrete changes in their lives. Now, this may be not true for OP--maybe he or she IS really "reorienting their career", but I'm simply saying that you need to have clarity in your mind first.
Last edited:
- Joined
- Nov 6, 2009
- Messages
- 427
- Reaction score
- 568
This is getting extremely off track. Would just say that this:
To turn it back to the topic of the thread, I'm not sure how we got on the topic of prestige. This isn't something I particularly care about nor do most of my colleagues (maybe it's different at other institutions), but I would agree with @SmallBird that much of the discouragement comes from not being able to provide what patients need (psychosocial interventions, a job, a house) and feeling like all we get paid to do is use our biological tools to address a tsunami of social problems that a sprinkling of escitalopram or even a good regimen of clozapine can't fix. Which probably prompts patient and policy maker frustration with our field, which prompts more people to leave, and around we go
is getting weirdly aggressive. I'm a health services researcher who writes grants to improve care for people with psychotic spectrum illnesses, but thank you for offering your services to have me pay to whine to you.I mean... Isn't it though? What use is it? Why should I waste my time listening to you whine about "the system" all day when I can use the same time to write another grant to actually do something about "the system"? Maybe I can get PAID to listen to you whine in a focus group instead--or be your THERAPIST and actually HELP you.
To turn it back to the topic of the thread, I'm not sure how we got on the topic of prestige. This isn't something I particularly care about nor do most of my colleagues (maybe it's different at other institutions), but I would agree with @SmallBird that much of the discouragement comes from not being able to provide what patients need (psychosocial interventions, a job, a house) and feeling like all we get paid to do is use our biological tools to address a tsunami of social problems that a sprinkling of escitalopram or even a good regimen of clozapine can't fix. Which probably prompts patient and policy maker frustration with our field, which prompts more people to leave, and around we go
Not here for the prestige. Don't care.It's not always low prestige. Prestige is associated with exclusivity, expensiveness, and the demand of people who can pay. It's not associated with necessity.
Plenty of psychotherapists (and not just MDs) have exclusive, expensive, and high-demand practices. They just don't address issues relating to people who can't afford their services.
There is NOT a single service that aims towards public welfare and the indigent that's considered high prestige, not now, not in history, not in any other culture. That's literally the definition of prestige. People need to clarify their thoughts. People equate virtue with prestige. Many jobs relating to public welfare are *necessary* and *virtuous*, and *valuable*, but they aren't "prestigious". There are jobs that very obviously are both virtuous and prestigious, many are in medicine (transplant surgery, etc). High-end practices in psychiatry that are very specialized in technical expertise (i.e. pediatric psychopharmacologists) likely fall into this category, but the judgment call here is not nearly as obvious. Similar things exist in psychotherapy (specialized psychotherapists for say, athletes). This dynamic is not limited to mental health. This is a feature of the entire "capitalist" system. So you say okay I would rather reform the system at large so that I make sure that people who specialized high demand services cap their fees so that poor people who also need it can get access to it. This basically is what happened in communist countries. It doesn't work. Brute force centralized organization of supply and demand never works.
This is not to say that the current mental health system is perfect. Not at all. My point is that the systems-level issues are very specific and detail driven, and when you talk in personal, emotional, and philosophical terms, you suppress actual productive discussion of actual problems that are treatable via policy interventions. And you need to have a more definable clarity in thinking: do you really care about "the system" or do you just want to get a new job? In general, I find that people who complain about "the system" really just want a new job but use "the system" as a post hoc justification for making concrete changes in their lives. Now, this may be not true for OP--maybe he or she IS really "reorienting their career", but I'm simply saying that you need to have clarity in your mind first.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
To turn it back to the topic of the thread, I'm not sure how we got on the topic of prestige. This isn't something I particularly care about nor do most of my colleagues (maybe it's different at other institutions), but I would agree with @SmallBird that much of the discouragement comes from not being able to provide what patients need (psychosocial interventions, a job, a house) and feeling like all we get paid to do is use our biological tools to address a tsunami of social problems that a sprinkling of escitalopram or even a good regimen of clozapine can't fix. Which probably prompts patient and policy maker frustration with our field, which prompts more people to leave, and around we go
You can easily provide what patients need in a different treatment context that carries more prestige, which then attracts demand of people who can afford what "people need", which is why this question of prestige came into existence.
What do you think I do all day in a fancy private practice? It's no more than psychotherapy, getting people a job, getting them a house, etc. etc. I know I'm doing a great job, but I also know that I'm exclusive. Your problem is that you are trying to solve a problem that has no solution. You can't build a system where you have exclusivity but also demand that people don't pay for it. That's an economic impossibility.
People leave public psychiatry because it's not "prestigious" enough in lay terms (not pay enough, doesn't command enough "respect", has a poor lifestyle, etc). So if you really go down to "the root cause", you'd have to be more honest about what is REALLY happening here.
And I'm not being aggressive. I'm being honest. Unfortunately, in this world honesty can be misinterpreted as aggression. I also disagree that you don't care about prestige. The job you have (as a researcher, instead of a strict clinician) is considered more "prestigious" for a variety of reasons, and you and I both know this. And the reason for that is that your job is one that's more MBA-like. Secondarily, in general, people who are in these types of positions are able to "make it" because of other factors (family money, etc), so you kind of have to solve that whole basket of problems... You can AFFORD to not "care" about some aspects of prestige (i.e. money), but this unfortunately is not universal for people who complain about their jobs in public psychiatry.
Not here for the prestige. Don't care.
Yes, but the problem you raise relates to the system. I'm telling you that the reason that you can't find a therapist who does behavioral activation is that that is not "prestigious". But then you tell me you don't care about prestige. LOL There is a misalignment here, as you said. The misalignment is that your personal virtue can't overcome the system's resistance.
Last edited:
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
lol, how did a discussion about efficacy of psychiatric interventions turn to 'prestige'. I guess the answer is obvious.
I hope people like @dl2dp2 are no where near the leadership, because if this is how decisions are made.....
As for the thread, working in am employed position in a system will always be taxing and draining to an extent.
It is not the most pleasant type of work, but one has to do what one has to do. I could never do that full time.
I hope people like @dl2dp2 are no where near the leadership, because if this is how decisions are made.....
As for the thread, working in am employed position in a system will always be taxing and draining to an extent.
It is not the most pleasant type of work, but one has to do what one has to do. I could never do that full time.
- Joined
- Sep 3, 2022
- Messages
- 647
- Reaction score
- 1,364
My biggest complaint is that 1/4 of my intakes are people wanting inappropriate access to benzos/stimulants, becoming infuriated when they dont get what they want, because I have to be the one to stay no, and then they destroy me on patient reviews that the clinic pushes hard. We give people that often have low intelligence/insight and poor judgement a voice to complain with the goal of improving customer service, but focus on the superficial aspects. We dont focus on the objective parts. This is the way mental health is headed towards, where the patient "is always right". More and more psychiatrists will want to stop working with these cases because of the burn out and then the shortage will only get worse.
- Joined
- Nov 30, 2009
- Messages
- 4,236
- Reaction score
- 9,209
No one else is talking about "prestige" which is irrelevant to this conversation. People don't leave public psychiatry because it's not "prestigious" (if they cared about that they would never have worked in that field in the first place). There are two types of people who do public psych - those who have a deep desire to help the most marginalized and disenfranchised communities, and those that can't get other jobs. The former do not care about external validation because they find great meaning and purpose in their work. The latter are bottom of the barrel and don't have the luxury of considering it. People leave public psychiatry because of some of the challenges that smallbird describes - the frustrations and moral injury that come from trying to serve a population to the best of one's abilities but not having the resources (which are usually not medical in nature) to do so.People leave public psychiatry because it's not "prestigious" enough in lay terms (not pay enough, doesn't command enough "respect", has a poor lifestyle, etc). So if you really go down to "the root cause", you'd have to be more honest about what is REALLY happening here.
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
No one else is talking about "prestige" which is irrelevant to this conversation. People don't leave public psychiatry because it's not "prestigious" (if they cared about that they would never have worked in that field in the first place). There are two types of people who do public psych - those who have a deep desire to help the most marginalized and disenfranchised communities, and those that can't get other jobs. The former do not care about external validation because they find great meaning and purpose in their work. The latter are bottom of the barrel and don't have the luxury of considering it. People leave public psychiatry because of some of the challenges that smallbird describes - the frustrations and moral injury that come from trying to serve a population to the best of one's abilities but not having the resources (which are usually not medical in nature) to do so.
I would add that lots of people attracted to leadership positions go to public psychiatry.
It's useless to generalize, but in my experience, it absolutely can lead to name recognition and political influence (of some sort).
- Joined
- Sep 3, 2022
- Messages
- 647
- Reaction score
- 1,364
People leave public psychiatry because of some of the challenges that smallbird describes - the frustrations and moral injury that come from trying to serve a population to the best of one's abilities but not having the resources (which are usually not medical in nature) to do so.
that is exactly why i left my first job in the community setting. often in these jobs your role is to compensate for the lack of providers/trained staff, and you actually end up doing 3 in 1 jobs but barely get paid for 1 job. The ancillary staff often dont want to be there, your lucky if the EMR isnt from 60 years ago, your schedule is >20 people a day and there is always a chance that a disgruntled patient will attack you. Its a shame because i liked the patients but the logistics were just awful and the admin were incompetent and in complete denial at that job so they were determined to keep things "status quo"
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
lol, how did a discussion about efficacy of psychiatric interventions turn to 'prestige'. I guess the answer is obvious.
I hope people like @dl2dp2 are no where near the leadership, because if this is how decisions are made.....
Too late. People "like me" have already been in leadership for the last 30 years. Look at Tom Insel. Look at all the chairs of major departments. Look at the leading journals. Look at the *RESIDENTS* major departments hire. LOL. Again, as an insider, I'm simply explaining the mechanism that people find so mysterious... It's very confusing as to WHY plenty of effective interventions don't get funding. I'm explaining this to you. We can broaden the topic and more about details in pharmaceutical development, but that would be even more "off topic"...
Disagree there. I agree a lot of people in public psychiatry get there FIRST because they had youthful idealism in finding meaning and purpose in their work. Once they get there they find that the work is not at all what they thought it was, and leave for "more prestigious" pastures. So then people who stay are truly "the bottom of the barrel" (as you claim ever so kindly), which admins have problem differentiating between MDs and NPs. What I think you mean here is that a lot of people who are stuck in that system have personal problems themselves, which in the collective prevents things from going in a certain optimal direction.No one else is talking about "prestige" which is irrelevant to this conversation. People don't leave public psychiatry because it's not "prestigious" (if they cared about that they would never have worked in that field in the first place). There are two types of people who do public psych - those who have a deep desire to help the most marginalized and disenfranchised communities, and those that can't get other jobs. The former do not care about external validation because they find great meaning and purpose in their work. The latter are bottom of the barrel and don't have the luxury of considering it. People leave public psychiatry because of some of the challenges that smallbird describes - the frustrations and moral injury that come from trying to serve a population to the best of one's abilities but not having the resources (which are usually not medical in nature) to do so.
I understand the frustration perfectly well--my work dovetails a lot with that system. I am simply saying that you need to make a decision in your life about where you want to go. You either leave or try to change the system in some very incremental/specific ways, which is a tedious process.
That sounds very frustrating, and is exactly what I am getting at. Quality improvement and performance measures are often tied to things like this as well.My biggest complaint is that 1/4 of my intakes are people wanting inappropriate access to benzos/stimulants, becoming infuriated when they dont get what they want, because I have to be the one to stay no, and then they destroy me on patient reviews that the clinic pushes hard. We give people that often have low intelligence/insight and poor judgement a voice to complain with the goal of improving customer service, but focus on the superficial aspects. We dont focus on the objective parts. This is the way mental health is headed towards, where the patient "is always right". More and more psychiatrists will want to stop working with these cases because of the burn out and then the shortage will only get worse.
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
Too late. People "like me" have already been in leadership for the last 30 years. LOL. Again, as an insider, I'm simply explaining the mechanism that people find so mysterious... It's very confusing as to WHY plenty of effective interventions don't get funding. I'm explaining this to you. We can broaden the topic and more about details in pharmaceutical development, but that would be even more "off topic"...
But we know that. You don't need to 'explain' anything.
It's what posters already explained above. There is a bias for drugs because this is how you pump $$ in the field. It's not rocket science.
You just came here and tried to justify those decisions.
But I also think the idea that promoting psychosocial interventions will somehow diminish your status as a physician is bs. No one is saying to dump the drugs. Antipsychotics clearly do lots of work. Just that it's not the most sensible pathway to invest resources this way when there are more obvious political interventions that will likely be higher yield.
Physician burnout is also not exactly 'high prestige'. LOL.
Yes, as stated, the fact that power remains in the hands of those who perpetuate the injurious circumstances adds insult to injury. I hope it will change.Too late. People "like me" have already been in leadership for the last 30 years. Look at Tom Insel. Look at all the chairs of major departments. Look at the leading journals. Look at the *RESIDENTS* major departments hire. LOL. Again, as an insider, I'm simply explaining the mechanism that people find so mysterious... It's very confusing as to WHY plenty of effective interventions don't get funding. I'm explaining this to you. We can broaden the topic and more about details in pharmaceutical development, but that would be even more "off topic"...
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
But we know that. You don't need to 'explain' anything.
It's what posters already explained above. There is a bias for drugs because this is how you pump $$ in the field. It's not rocket science.
You just came here and tried to justify those decisions.
But I also think the idea that promoting psychosocial interventions will somehow diminish your status as a physician is bs. No one is saying to dump the drugs. Antipsychotics clearly do lots of work. Just that it's not the most sensible pathway to invest resources this way when there are more obvious political interventions that will likely be higher yield.
Physician burnout is also not exactly 'high prestige'. LOL.
It's not a justification. It's a mechanism. If you don't pump $$ into a field, nothing gets done. And people are unwilling to dump $$ into a field unless it's technical, exclusive, high prestige.
I also don't dispute that a lot of it requires some sort of political process. But do you actually KNOW what this process involves? Do you do this for a living (like I do), and how many players are involved in this process? I'm explaining to you why this process is complicated and giving you a taste of what it's like to actually have to sit down and solve a problem. It's a useful exercise to scrutinize what a DHHS grant or a state statutory implementation package looks like. When I talk to clinicians in the field, so far very very few people have an actual desire to do this kind of work, especially when it would cut their pay.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
Yes, as stated, the fact that power remains in the hands of those who perpetuate the injurious circumstances adds insult to injury. I hope it will change.
You should make decisions pertaining to your career development with the assumption that it will never change. In any case, even if it changes the pacing would be slow and uneven.
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
It's not a justification. It's a mechanism. If you don't pump $$ into a field, nothing gets done. And people are unwilling to dump $$ into a field unless it's technical, exclusive, high prestige.
I also don't dispute that a lot of it requires some sort of political process. But do you actually KNOW what this process involves? Do you do this for a living (like I do), and how many players are involved in this process? I'm explaining to you why this process is complicated and giving you a taste of what it's like to actually have to sit down and solve a problem. It's a useful exercise to scrutinize what a DHHS grant or a state statutory implementation package looks like. When I talk to clinicians in the field, so far very very few people have an actual desire to do this kind of work, especially when it would cut their pay.
Well, you wanted to give psychiatry a blueprint of how to become the new derm. So your posts here aren't merely descriptive.
And right, money will go to what appears like is technical, scientific and exclusive, and much of it across the years in psychiatry has been snake oil.
But I also dispute the idea that your salary as a system employed psychiatrist will go down because we should be doing the sensible and logical thing (giving more weight to psychosocial interventions).
I also don't think this will get solved by telling physicians to write grants.
This is a political issue. And spreading awareness and political mobilization is EXACTLY how you start to address it.
Last edited:
- Joined
- Sep 3, 2022
- Messages
- 647
- Reaction score
- 1,364
yep, even if we know the reviews are BS, it doesnt matter. If a patient presents to to their PCP asking for xanax, and PCP says "psych will prescribe". PCP isnt the one that gets the bad review, we do. You can count on being dinged on 25% of your intakes basically.That sounds very frustrating, and is exactly what I am getting at. Quality improvement and performance measures are often tied to things like this as well.
What has helped me some, is that i keep telling myself I will always do what I feel is the right thing to do and never compromise regardless of anything else. If a job doesnt like me because of it, then i suppose on to the next. Which would suck because I do like this job, but im viewing that morality is not worth the compromise for good reviews if it ever comes down to it. And also trying to build a decent nest egg financially in the meantime push comes to shove.
Ultimately i just really tell myself every day that I do what i can. People come with 1,000 problems and insane situations that I can just fix for them. We are limited and we cant work miracles sometimes. We also cant give people whatever they want for a good review, this isnt uber
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
Well, you wanted to give psychiatry a blueprint of how to become the new derm. So your posts here aren't merely descriptive.
And right, money will go to what appears like is technical, scientific and exclusive, and much of it across the years in psychiatry has been snake oil.
But I also dispute the idea that your salary as a system employed psychiatrist will go down because we should be doing the sensible and logical thing (given more weight to psychosocial interventions).
I also don't think this will get solved by telling physicians to write grants.
This is a political issue. And spreading awareness is EXACTLY how you start to address it.
Sure, there's a normative element to it, but I think a large number of people in our field are on my side--a large number of young psychiatrists truly want to make psychiatry into the new derm--a cutting-edge, technical field that commands high prestige and salary with excellent lifestyle. I think it's futile to try to mishmash people of dramatically different career goals into the same specialty, which is why I think the specialty should be split via formal training pathways, which it is already doing and in my mind a positive turn.
In terms of physicians writing grants--if you want to solve the problem, you kind of have to. Physicians who actually run CMHCs instead of merely being employees by definition write grants. You can spread awareness more, but I think that actually has a negative impact. You make it sound like the jobs in public psychiatry are constrained in a way that cannot be improved except via mass political action (at what? APA that's overtaken by biological psychiatrists and pharma? state and federal legislature? nonprofits? Let's be more concrete here and actually have deliverables...) at an uncertain timeline. I'm saying, no you are wrong. Learn to write grants and appreciate how funding streams for the services you advocate actually come to fruition. But then you tell me this is not the physician's job. You pigeonhole yourself into a dead-end of impossibilities. I don't know what to tell you here.
Last edited:
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
Sure, there's a normative element to it, but I think a large number of people in our field are on my side. I think it's futile to try to mishmash people of dramatically different career goals into the same specialty, which is why I think the specialty should be split via formal training pathways, which it is already doing and in my mind positive.
In terms of physicians writing grants--if you want to solve the problem, you kind of have to. Physicians who actually run CMHCs instead of merely being employees by definition write grants. You can spread awareness more, but I think that actually has a negative impact. You make it sound like the jobs in public psychiatry are constrained in a way that cannot be improved except via mass political action at an uncertain timeline. I'm saying, no you are wrong. Learn to write grants and appreciate how funding streams for the services you advocate actually come to fruition. But then you tell me this is not the physician's job. You pigeonhole yourself into a dead-end of impossibilities. I don't know what to tell you here.
The biggest roadblock is not scarcity of grant submissions, but who approves them and who grants the money i.e political action and leadership. Both in psychiatry and on the public level.
You address this through political mobilization. Both among psychiatrists and the general public.
You also seem confused as to whether you're telling us how it is, or how it should be (clearly the latter imo).
I think your 'solutions' are far less fruitful than the 'whining' you're complaining about.
It's a bit absurd as well to claim that every psychiatrist needs to be submitting a grant to have a voice in how their clinical day to day work is going.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
You address this through political mobilization. Both among psychiatrists and the general public.
You also seem confused as to whether you're telling us how it is, or how it should be (clearly the latter imo).
I think your 'solutions' are far less fruitful than the 'whining' you're complaining about.
Sure, I don't disagree on principle at all on these points.
In actuality, nobody wants to do this work (political mobilization). First of all, you have to raise money. LOL. This brings us right back to a discussion of prestige, writing strategic plans, dealing with 30 players with different priroities, blah blah, etc.
As someone who actually was involved in a fairly substantial campaign recently, yeah... there's a reason why political work is done by the already rich.
No worries, plenty of good thoughts on this thread.I don't know what to tell you here.
- Joined
- Oct 13, 2008
- Messages
- 4,154
- Reaction score
- 7,957
A lot in this thread, some very thought-provoking, some ... okay, @dl2dp2 , you are more successful and more connected and smarter and richer than all of us. You are also more attractive and a better dresser and are more sophisticated and discerning in your tastes. Are you satisfied?
In general I regard the output of Pharma with intense, Cartesian levels of skepticism. But if we really end up with a muscarinic agonist that is even middlingly effective for schizophrenia that would be huge. Mostly in terms of reducing the incidence of metabolic syndrome and CVD in our patient population. I'm not convinced that is what we are going to get, but it wouldn't be nothing.
Setting aside the prestige nonsense (if you think nowhere ever in history has there been alignment between working on behalf of the indigent and prestige, the history of the Catholic Church may want to have a word with you), I do agree that making the field focused in psychosocial interventions primarily raises the question I have nattered on about before. If we are not primarily doing things that are clearly medical, why exactly should we have special role or authority as physicians? I still have never received a good answer to this. In that much at least I do agree that making us a mostly psychosocial field would make it even easier for us to be replaced.
In general I regard the output of Pharma with intense, Cartesian levels of skepticism. But if we really end up with a muscarinic agonist that is even middlingly effective for schizophrenia that would be huge. Mostly in terms of reducing the incidence of metabolic syndrome and CVD in our patient population. I'm not convinced that is what we are going to get, but it wouldn't be nothing.
Setting aside the prestige nonsense (if you think nowhere ever in history has there been alignment between working on behalf of the indigent and prestige, the history of the Catholic Church may want to have a word with you), I do agree that making the field focused in psychosocial interventions primarily raises the question I have nattered on about before. If we are not primarily doing things that are clearly medical, why exactly should we have special role or authority as physicians? I still have never received a good answer to this. In that much at least I do agree that making us a mostly psychosocial field would make it even easier for us to be replaced.
G Sheb
Full Member
- Joined
- Jan 1, 2022
- Messages
- 405
- Reaction score
- 664
A lot in this thread, some very thought-provoking, some ... okay, @dl2dp2 , you are more successful and more connected and smarter and richer than all of us. You are also more attractive and a better dresser and are more sophisticated and discerning in your tastes. Are you satisfied?
In general I regard the output of Pharma with intense, Cartesian levels of skepticism. But if we really end up with a muscarinic agonist that is even middlingly effective for schizophrenia that would be huge. Mostly in terms of reducing the incidence of metabolic syndrome and CVD in our patient population. I'm not convinced that is what we are going to get, but it wouldn't be nothing.
Setting aside the prestige nonsense (if you think nowhere ever in history has there been alignment between working on behalf of the indigent and prestige, the history of the Catholic Church may want to have a word with you), I do agree that making the field focused in psychosocial interventions primarily raises the question I have nattered on about before. If we are not primarily doing things that are clearly medical, why exactly should we have special role or authority as physicians? I still have never received a good answer to this. In that much at least I do agree that making us a mostly psychosocial field would make it even easier for us to be replaced.
But social interventions will not replace clozapine, lithium or the monthly haldol shot.
They will not replace starting an antipsychotic after a FEP hospitalization.
They will not replace almost any of the work that we already do.
There is probably more 'niche' work in psychiatry in SMI and acute psychiatry than in any other field of psychiatry. Ironically, much more so than the 'snake oil' that gets sold to the worried well by Columbia and Harvard grads.
The issue is more that our resources are unbalanced because there will always big pharma knocking on the door to sell its next product instead of sensibly using our resources to help patients connect with their families, have a roof over their heads and the daily organization they need to lead a dignified life. Interventions that are just as critical as the antipsychotics.
I do not see where that fear is coming from.
- Joined
- Sep 3, 2022
- Messages
- 647
- Reaction score
- 1,364
Physicians who actually run CMHCs instead of merely being employees by definition write grants. You can spread awareness more, but I think that actually has a negative impact. You make it sound like the jobs in public psychiatry are constrained in a way that cannot be improved except via mass political action (at what? APA that's overtaken by biological psychiatrists and pharma? state and federal legislature? nonprofits? Let's be more concrete here and actually have deliverables...) at an uncertain timeline. I'm saying, no you are wrong. Learn to write grants and appreciate how funding streams for the services you advocate actually come to fruition. But then you tell me this is not the physician's job. You pigeonhole yourself into a dead-end of impossibilities. I don't know what to tell you here.
Do physicians actually run CMHCs? The majority ive seen are run by some idiot with a bachelors degree from university of phoenix. I think typically board of directors, CEOs, admin for CMHCs from what ive seen are non clinical people.
- Joined
- Jun 6, 2016
- Messages
- 770
- Reaction score
- 906
A brilliant psychiatrist once told me “doing the right thing is really hard sometimes but it is still the right thing to do.” I often think of that line. It doesn’t make it easier but reinforces my resolve.yep, even if we know the reviews are BS, it doesnt matter. If a patient presents to to their PCP asking for xanax, and PCP says "psych will prescribe". PCP isnt the one that gets the bad review, we do. You can count on being dinged on 25% of your intakes basically.
What has helped me some, is that i keep telling myself I will always do what I feel is the right thing to do and never compromise regardless of anything else. If a job doesnt like me because of it, then i suppose on to the next.
.
Well, things develop over time and don't get redesigned by a master planner on the basis of a new insight. The field should develop in a way that makes sense for our patients but that won't overnight change our training pathways or ways staffing is structured. Like when the marines were started their function was highly distinct from the army and navy but that has changed over time and if you wanted the most efficient plan and started from scratch you might not have a seperate branch. But they do a good job and are heavily entrenched and so aren't going anywhere.A lot in this thread, some very thought-provoking, some ... okay, @dl2dp2 , you are more successful and more connected and smarter and richer than all of us. You are also more attractive and a better dresser and are more sophisticated and discerning in your tastes. Are you satisfied?
In general I regard the output of Pharma with intense, Cartesian levels of skepticism. But if we really end up with a muscarinic agonist that is even middlingly effective for schizophrenia that would be huge. Mostly in terms of reducing the incidence of metabolic syndrome and CVD in our patient population. I'm not convinced that is what we are going to get, but it wouldn't be nothing.
Setting aside the prestige nonsense (if you think nowhere ever in history has there been alignment between working on behalf of the indigent and prestige, the history of the Catholic Church may want to have a word with you), I do agree that making the field focused in psychosocial interventions primarily raises the question I have nattered on about before. If we are not primarily doing things that are clearly medical, why exactly should we have special role or authority as physicians? I still have never received a good answer to this. In that much at least I do agree that making us a mostly psychosocial field would make it even easier for us to be replaced.
- Joined
- Oct 13, 2008
- Messages
- 4,154
- Reaction score
- 7,957
Well, things develop over time and don't get redesigned by a master planner on the basis of a new insight. The field should develop in a way that makes sense for our patients but that won't overnight change our training pathways or ways staffing is structured. Like when the marines were started their function was highly distinct from the army and navy but that has changed over time and if you wanted the most efficient plan and started from scratch you might not have a seperate branch. But they do a good job and are heavily entrenched and so aren't going anywhere.
Sure, path dependence is a thing. But why not just turn it over even more to social workers? Why hire MDs at all?
I absolutely agree with you that many times our patients' needs are things that will never, ever, ever be fixed with medications. I just don't see why we would expect physicians qua physicians to be the ones fixing it.
- Joined
- Oct 13, 2008
- Messages
- 4,154
- Reaction score
- 7,957
But social interventions will not replace clozapine, lithium or the monthly haldol shot.
They will not replace starting an antipsychotic after a FEP hospitalization.
They will not replace almost any of the work that we already do.
There is probably more 'niche' work in psychiatry in SMI and acute psychiatry than in any other field of psychiatry. Ironically, much more so than the 'snake oil' that gets sold to the worried well by Columbia and Harvard grads.
The issue is more that our resources are unbalanced because there will always big pharma knocking on the door to sell its next product instead of sensibly using our resources to help patients connect with their families, have a roof over their heads and the daily organization they need to lead a dignified life. Interventions that are just as critical as the antipsychotics.
I do not see where that fear is coming from.
Oh, I'm not especially scared that we're actually going to focus more on solving the social determinants of health than fancy new drugs, the economic incentives are all wrong. And I prescribed lithium frequently and have multiple patients on clozapine and LAIs. So obviously I'm not giving up on the meds anytime soon.
I just think there is something to the idea that the winning move (and the one that makes more sense given how f'ing long our training pathway is) would be to have us as MDs focus more on highly specialized, technical skills. The biopsychosocial model is a) true and b) a terrible model in terms of clinical utility as it basically just throws up its hands and says "s**t is complicated, you figure it out." You make progress by picking pieces to focus on as a profession, just like family lawyers are not actually the same as couples therapists.
- Joined
- May 20, 2010
- Messages
- 5,310
- Reaction score
- 6,939
To say nothing of peer support, supported employment, family psychoeducation, and other evidence based practices found to reduce psychosis relapse in the RAISE trial as well as in other meta-analyses: Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis
And of course this is even more true outside of psychosis where psychotherapies have equal or greater effect sizes than medications.
I'm frankly befuddled by this post.
You realize that metanalysis is basically looking at psychosocial interventions on top of medication? It's not exactly making an argument that you can replace medication with any of those psychological or social support interventions. I mean, I don't think this is a particularly debated topic that SOME kind of psychosocial support is better than no support in patients with severe mental illness.
hippopotamusoath
Full Member
- Joined
- Nov 13, 2022
- Messages
- 49
- Reaction score
- 106
As they say--we can train any monkey to do surgery, the important thing is knowing when not to operate. In the same way, I think we do have a special authority in the sense that we have a deeper knowledge and broader context than just about anybody else in the mental health game. I can say with some confidence when something is or is not a prescription drug problem. I have worked with many excellent social workers and therapists who have never set foot on an inpatient unit, who have never seen severe and incapacitating psychosis, and who have a hard time differentiating between a psychotic BPD patient vs. someone with a genuine primary psychotic disorder.A lot in this thread, some very thought-provoking, some ... okay, @dl2dp2 , you are more successful and more connected and smarter and richer than all of us. You are also more attractive and a better dresser and are more sophisticated and discerning in your tastes. Are you satisfied?
In general I regard the output of Pharma with intense, Cartesian levels of skepticism. But if we really end up with a muscarinic agonist that is even middlingly effective for schizophrenia that would be huge. Mostly in terms of reducing the incidence of metabolic syndrome and CVD in our patient population. I'm not convinced that is what we are going to get, but it wouldn't be nothing.
Setting aside the prestige nonsense (if you think nowhere ever in history has there been alignment between working on behalf of the indigent and prestige, the history of the Catholic Church may want to have a word with you), I do agree that making the field focused in psychosocial interventions primarily raises the question I have nattered on about before. If we are not primarily doing things that are clearly medical, why exactly should we have special role or authority as physicians? I still have never received a good answer to this. In that much at least I do agree that making us a mostly psychosocial field would make it even easier for us to be replaced.
I would love to have the ability to divert a big chunk of my panel towards robust psychosocial interventions, and spend more of my time on the patients with truly medical issues.
- Joined
- Jan 5, 2002
- Messages
- 2,909
- Reaction score
- 2,941
A lot in this thread, some very thought-provoking, some ... okay, @dl2dp2 , you are more successful and more connected and smarter and richer than all of us. You are also more attractive and a better dresser and are more sophisticated and discerning in your tastes. Are you satisfied?
lol, this reminds me of The White Lotus. You have to admit, I make very valid points by subjecting the conventional narrative to downright honest scrutiny. So you look at someone successful and you say what is going on here, and then you say okay which part of this is fake and which is real? I'm not anything particular personally, though admittedly I have *seen* a lot. I *know* a lot of *stuff*, doesn't mean that I'm smarter or richer, and that's irrelevant anyway on a personal level. I'm saying I'm sort of a Morpheus of The Matrix if you will, I can start to get people to see the REALITY for what it is so everyone can make a choice as to whether they want to stay in the Matrix or get out of it.
This is also not particularly limited to me personally. I learned a lot from colleagues both junior and senior and I can see where things are coming from, and a lot of them have moe insight to specific topical issues than I do.
The point of all of this isn't to put people on some kind of bell curve and grade people and somehow assert my superiority. It's to say that you have options, you can do this and that, and choices have consequences. If you aren't happy, make a change.
Similar threads
- Replies
- 3
- Views
- 1K
