- Joined
- Aug 8, 2014
- Messages
- 216
- Reaction score
- 50
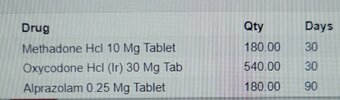
I have some Mehthadone patients I've inherited on like 10 TID for years no ekg and in general don't need to be on high opioids if at all.
I'm trying to clean it up. What is the dose limit you guys are using for Metha done? I've read and calculated one day 10mg BID to be the absolute max in terms of adhering to CDC guidelines.
Methadone has a disproportionately high amount of complications related to it.
Also how are you guys weaning these patients?
I'm trying to clean it up. What is the dose limit you guys are using for Metha done? I've read and calculated one day 10mg BID to be the absolute max in terms of adhering to CDC guidelines.
Methadone has a disproportionately high amount of complications related to it.
Also how are you guys weaning these patients?