He has undergone 4 MRI's since SRS and it doesn't appear to be recurrence. Cavity has small amount of stable enhancement along one edge that has minimally increased in size over those many months - just a tiny bit thicker. Unable to wean from Decadron 4mg QID since SRS either. If it is recurrence, it sure is taking its sweet time.
Wait... Small cavity, small stable enhancement, still on dex 4 mg QID ? Something is odd with that story. Was the initial tumor very large? I would have still expected the edema to have come down. What symptoms do they have and have they seen a neuro-oncologist? Those sorts of doses of dex long-term are pretty toxic.
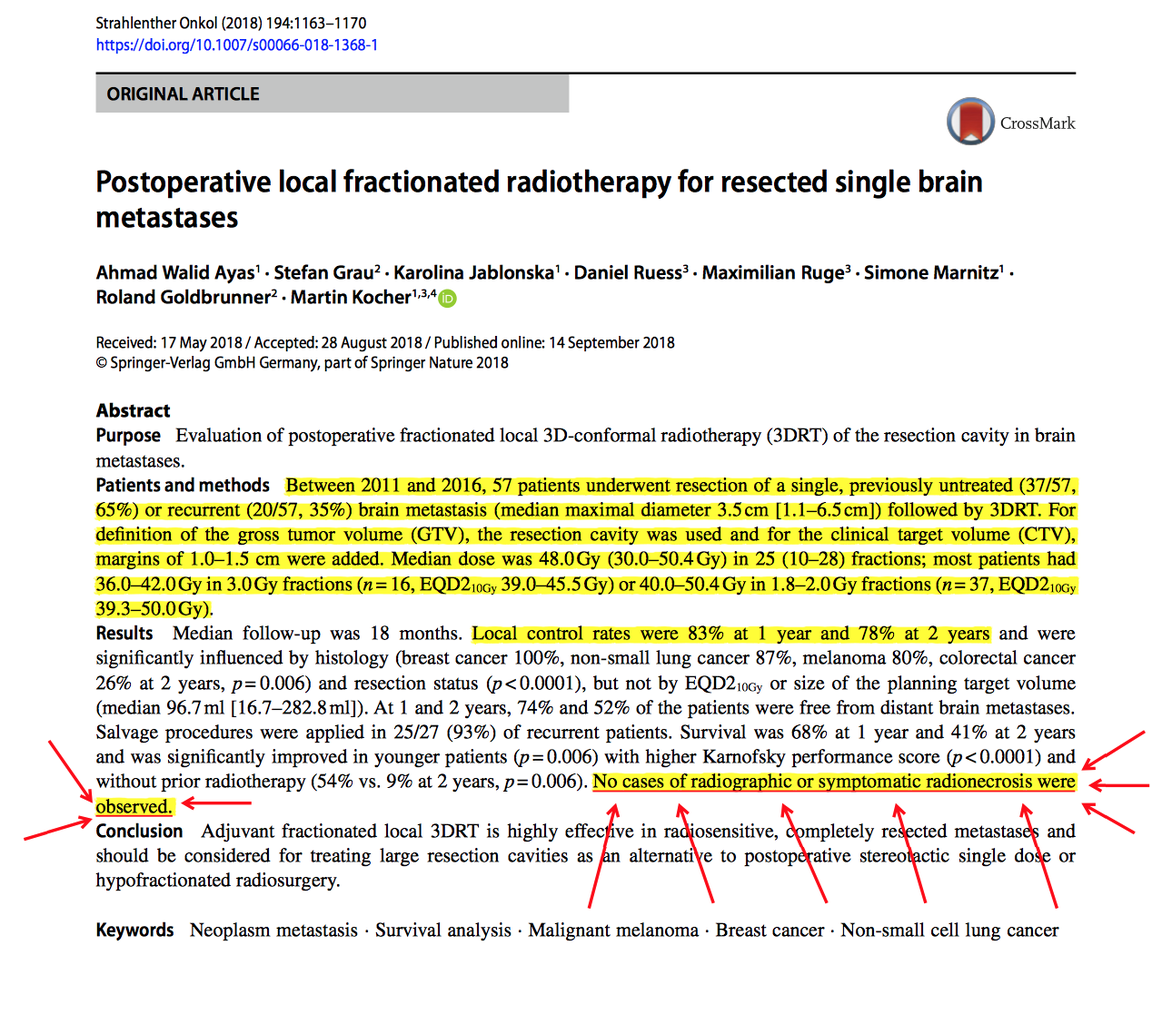
The correct dose, fractionation, margin, etc is debated significantly for cavities. If you poll the academic CNS people, you will get a lot of different answers to this question.
My thoughts are:
1. 40 Gy in 15 fractions to a focal area of the brain probably is safe. Some are trying to dose escalate that further for glioblastoma (there was a small European trial for this and some are proposing it in larger trials). Whether that's really effective in the brain mets setting, who knows. There is retrospective data for it.
2. Brain mets have always been thought of as a poor prognostic indicator (see survivals from the RPA which I'd argue is outdated), so there has always been a push for shorter courses of therapy. So could you do 10 fractions to 30-35 Gy or even 5 fractions 20 Gy focally? It's probably fine. Control is probably on the order of 15 Gy in 1 fraction for intact mets comparing different trials or series.
3. Stereotactic does pay better than a short 3D course, and even more when fractionated. I don't know how much that really plays into the decision making. Nevertheless, a lot of people feel very comfortable to deliver "stereotactic" courses with regular linac and mask setups and large PTVs to cavities, citing uncertainty about the target. More and more people are doing this for intact mets as well, which makes me nervous given the amount of thought that should go into stereotactic cases (and these used to go more to specialized centers).
4. For cavities with stereotactic alone, phase 3 data is from the MD Anderson trial (
Post-operative stereotactic radiosurgery versus observation for completely resected brain metastases: a single-centre, randomised, controlled, phas... - PubMed - NCBI). So I'm more apt to follow that. Their doses were on the lower side IMO--they had no RT necrosis and a high rate of failures for their ranges of doses (12 Gy - 16 Gy in 1 fraction), so I tend to push a little higher. For example, they had 3 protocol deviations for people giving 18 Gy in 1 fraction to small cavities, and I also tend to do this. Edit: I was also reminded of the NCCTG trial AKA RTOG 1270 by KHE88 below which used similar doses with 1 RT necrosis event.
5. Minnitti's data has been impressive for fractionated, especially three fraction. I wonder if it's "too good to be true" in their comparisons to single fraction. To answer the question, there is a cooperative trial coming soon for single fraction vs. fractionated for cavities (3 fraction for small, 5 fraction for large).
6. PTV margin is hotly debated. There is a question of technical accuracy depending on your linac setup and there is a question of subclinical spread. All of these tumors have microscopically positive margins, so you know there is still disease there. I tend to do 1 mm PTV on GK and 2 mm PTV on linac. There is a lot of variability in contouring, so at least we have the consensus paper as a starting point (
https://www.sciencedirect.com/science/article/pii/S0360301617339536?via=ihub).
As for doses, I treat 15 - 18 Gy in 1 fraction on GK for most cavities. For large cavities or tumors over 3 cm (or subtotal resection), I consider 30 Gy in 5 fractions on linac. Is this the right dose? Nobody really knows that either. The typical range of doses in 5 fractions is 25 - 35 Gy, with retrospective data you can pull to support any of those. There's also a cooperative group trial in the works on this question as well.

 link.springer.com
link.springer.com