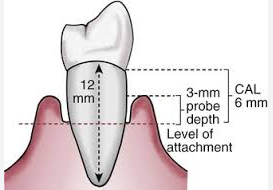
I've seen patients that have normal probing depths but they also have gingival recession. Here's an example where the probing depth is normal (3 mm) but there is 3 mm of recession. That corresponds to 6 mm of clinical attachment loss.
Referring to this table:
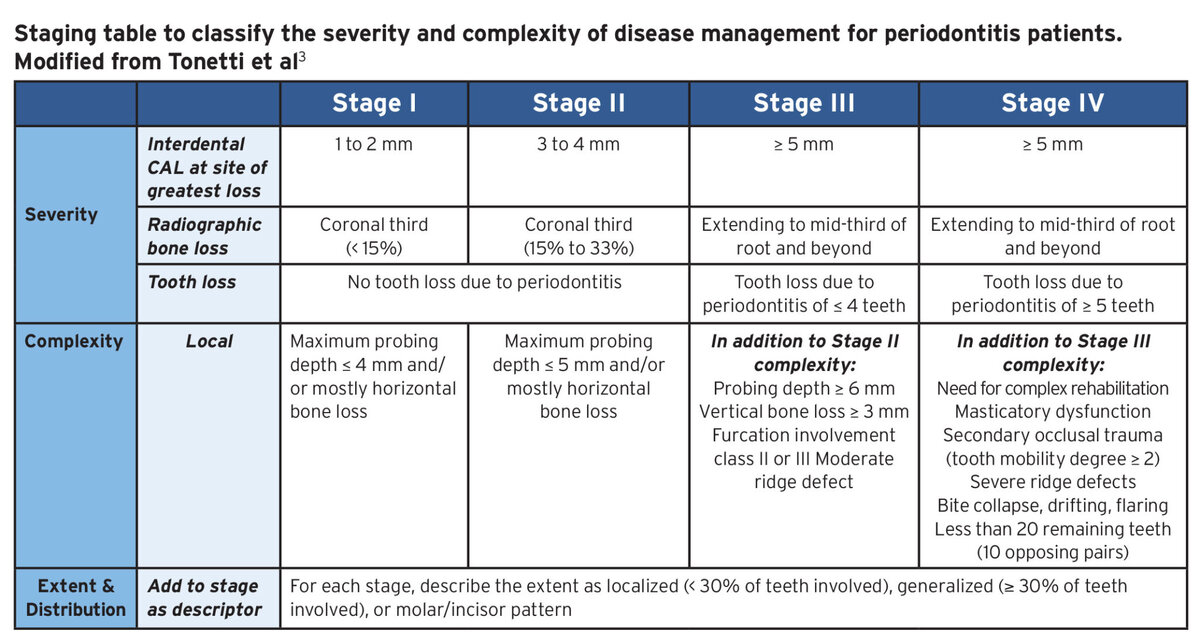
That example would be a Stage 3 if going by clinical attachment loss (6 mm) but a Stage 1 if going by probing depth (3 mm). With our office's software, entering the Stage number automatically determines the treatment plan. A Stage 1 treatment would be prophylaxis and a Stage 3 would be SRP. So how should this situation be classified? Would you go by probing depth or by clinical attachment loss? Can this still be considered a Stage 3 and treatment planned with SRP even if you don't observe much calculus?
Referring to this table:
That example would be a Stage 3 if going by clinical attachment loss (6 mm) but a Stage 1 if going by probing depth (3 mm). With our office's software, entering the Stage number automatically determines the treatment plan. A Stage 1 treatment would be prophylaxis and a Stage 3 would be SRP. So how should this situation be classified? Would you go by probing depth or by clinical attachment loss? Can this still be considered a Stage 3 and treatment planned with SRP even if you don't observe much calculus?