- Joined
- Nov 21, 1998
- Messages
- 12,576
- Reaction score
- 6,982
So happy this new technique was discovered to address an age-old scourge of humanity.
Pain Ther. 2022 Jun;11(2):655-665. doi: 10.1007/s40122-022-00385-x. Epub 2022 Apr 17.
Radiofrequency Ablation of the Superior Cluneal Nerve: A Novel Minimally Invasive Approach Adopting Recent Anatomic and Neurosurgical Data
O Visnjevac 1 2 3, M Pastrak 4, F Ma 2, T Visnjevac 2, A Abd-Elsayed 5
Affiliations expand
PMID: 35430676 PMCID: PMC9098737 DOI: 10.1007/s40122-022-00385-x
Free PMC article
Abstract
Objectives/introduction: Superior cluneal neuralgia (SCN) is a distinct cause of lower back and/or leg pain related to pathology of the superior cluneal nerve (SCn). SCN has been termed pseudo-sciatica and is an overlooked differential diagnosis when patients are otherwise presenting with low back and/or radicular pain. Radiofrequency ablation (RFA) is commonly used for denervation of the medial branches of the dorsal root for facet joint syndrome for sacroiliac joint; however, RFA has not been described to ablate the SCn for SCN. Herein, we present a novel interventional minimally invasive approach using RFA of the SCn for SCN in a series of 46 patients.
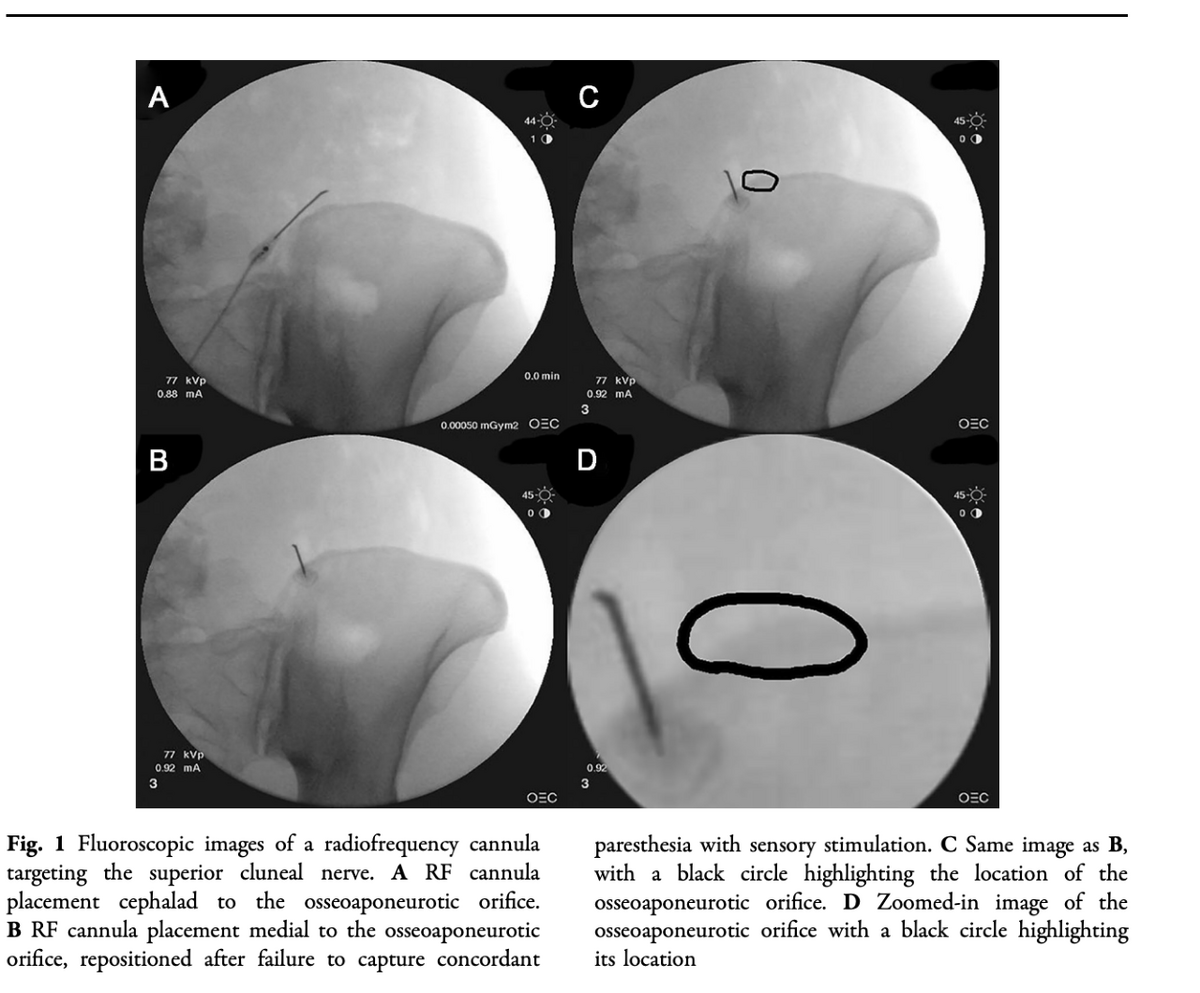
Methods: Institutional review board approved retrospective chart review was used to collect data for all SCn RFA cases from January 1, 2018, to February 8, 2021. Fluoroscopically guided SCn ablations were performed for patients with a positive "iliac crest point sign," reproductive of their back and leg pain during physical examination. Sensory stimulation was utilized to confirm RF cannula-probe placement adjacent to the SCn, and motor testing was used to confirm no distal motor response prior to monopolar RF ablation with a Halyard RF Generator (100 mm curved 22G 10 mm active tip RF cannulae). Charts were reviewed for time of analgesia follow-up, duration and degree of analgesia, improvements in patients' functional capacity, and changes in medication.
Results: Data were reviewed for 51 patients who underwent Scn RFA, 5 of which were lost to follow-up. The remaining 46 patients consisted of 29 women and 17 men with a mean age of 59.4 years; 78.3% (n = 36) had ongoing relief at a mean of 92.1 days follow-up, ranging from 13 to 308 days, with a mean of 92.3% analgesia (SD 15.0%). At a mean of 111.2 days of follow-up, ranging from 42-201 days, 21.7% (n = 10) of patients reported that their pain had returned and had 95% analgesia during that time period (SD 6.7%); 41.3% (n = 19) reported improved activity/gait, 17.4% reported improved mood (n = 8), and 8.7% reported decreased medication use (n = 4). Five patients had minor complications including bruising (1), 2-3 days of soreness on site (2), myofascial pain (1), and quadratus lumborus muscle spasm relieved with trigger point injection (1).
Conclusions: This is the first report of both technique and outcomes for radiofrequency ablation of superior cluneal neuralgia. This series suggests that RFA of the SCn is a suitable intervention for the treatment of SCN; 21.7% of patients reported a mean of 95% analgesia for a mean duration of 111.2 days, and the remaining 78.3% of patients reported ongoing relief with a mean of 92.3% analgesia at last follow-up (mean 92.1 days). There were no serious adverse events.
Keywords: Low back pain; Radiofrequency ablation; Superior cluneal nerve.
Pain Ther. 2022 Jun;11(2):655-665. doi: 10.1007/s40122-022-00385-x. Epub 2022 Apr 17.
Radiofrequency Ablation of the Superior Cluneal Nerve: A Novel Minimally Invasive Approach Adopting Recent Anatomic and Neurosurgical Data
O Visnjevac 1 2 3, M Pastrak 4, F Ma 2, T Visnjevac 2, A Abd-Elsayed 5
Affiliations expand
PMID: 35430676 PMCID: PMC9098737 DOI: 10.1007/s40122-022-00385-x
Free PMC article
Abstract
Objectives/introduction: Superior cluneal neuralgia (SCN) is a distinct cause of lower back and/or leg pain related to pathology of the superior cluneal nerve (SCn). SCN has been termed pseudo-sciatica and is an overlooked differential diagnosis when patients are otherwise presenting with low back and/or radicular pain. Radiofrequency ablation (RFA) is commonly used for denervation of the medial branches of the dorsal root for facet joint syndrome for sacroiliac joint; however, RFA has not been described to ablate the SCn for SCN. Herein, we present a novel interventional minimally invasive approach using RFA of the SCn for SCN in a series of 46 patients.
Methods: Institutional review board approved retrospective chart review was used to collect data for all SCn RFA cases from January 1, 2018, to February 8, 2021. Fluoroscopically guided SCn ablations were performed for patients with a positive "iliac crest point sign," reproductive of their back and leg pain during physical examination. Sensory stimulation was utilized to confirm RF cannula-probe placement adjacent to the SCn, and motor testing was used to confirm no distal motor response prior to monopolar RF ablation with a Halyard RF Generator (100 mm curved 22G 10 mm active tip RF cannulae). Charts were reviewed for time of analgesia follow-up, duration and degree of analgesia, improvements in patients' functional capacity, and changes in medication.
Results: Data were reviewed for 51 patients who underwent Scn RFA, 5 of which were lost to follow-up. The remaining 46 patients consisted of 29 women and 17 men with a mean age of 59.4 years; 78.3% (n = 36) had ongoing relief at a mean of 92.1 days follow-up, ranging from 13 to 308 days, with a mean of 92.3% analgesia (SD 15.0%). At a mean of 111.2 days of follow-up, ranging from 42-201 days, 21.7% (n = 10) of patients reported that their pain had returned and had 95% analgesia during that time period (SD 6.7%); 41.3% (n = 19) reported improved activity/gait, 17.4% reported improved mood (n = 8), and 8.7% reported decreased medication use (n = 4). Five patients had minor complications including bruising (1), 2-3 days of soreness on site (2), myofascial pain (1), and quadratus lumborus muscle spasm relieved with trigger point injection (1).
Conclusions: This is the first report of both technique and outcomes for radiofrequency ablation of superior cluneal neuralgia. This series suggests that RFA of the SCn is a suitable intervention for the treatment of SCN; 21.7% of patients reported a mean of 95% analgesia for a mean duration of 111.2 days, and the remaining 78.3% of patients reported ongoing relief with a mean of 92.3% analgesia at last follow-up (mean 92.1 days). There were no serious adverse events.
Keywords: Low back pain; Radiofrequency ablation; Superior cluneal nerve.

