- Joined
- Aug 8, 2014
- Messages
- 216
- Reaction score
- 50
Hey All,
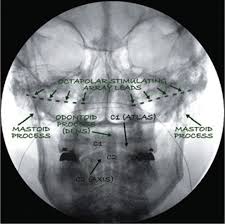
Has anyone here done a peripheral nerve stimulator for Occipital Neuralgia? I have a patient who has done every medical and almost every interventional option for his occipital neuralgia as well as seen tons of academic headache specialists. Nothing has worked. The only thing that has worked are Occipital nerve blocks at the ridge which provide temporary but profound relief (on the order of days to weeks). TON C3/4 Rhizotomies/blocks haven't worked either. So the other day I trialed a PNS stimulator and placed the leads at the bilateral occipital ridges kind of like this picture below (not my actual patient's picture).
It went very well. The patient had >95% relief for one week of the trial and tells me he still feels like he has some residual benefit from the trial. He was so happy. He was in tears at the follow up post op. He is really looking forward to the implant.
The problem is the company I'm using has a small IPG that I have to figure out where to put and how to tunnel it. I have several concerns and because of these concerns I may refer out or just refer to a neurosurgeon who does this but he puts the stimulator at C2 (NOT where I trialed and had major success), or maybe send to surgery for decompression.
1. I've never done one of these but it seemed easy enough to trial. I am a little concerned about the implant because I don't know a good place to place the IPG (albiet being tiny and thing. It is with mainly with this company because this is the only one my ASC approved). I am concerned about lead migration because its in the neck- an area with so much mobility.
2. It is technically considered "off-label" use of the device and I have never done one before. I don't really know anyone in my area who does much of this. I am concerned that in the event something goes wrong both of those situations can be used against me. I would like to see one being done but I don't know anyone else near me that does this.
3. The skin near the occipital ridge and the superior neck does not have much fat and so I think tunneling might be difficult.
4. Should I just NOT do this with this company and wait till my ASC approves the PNS company that does not have an IPG to tunnel to (Like StimWave)?
My main two concerns are IPG placement/tunneling as well as the technical off label use.
I really want this to work out for this patient because he is desperate has been dealing with this since being a teenager and he tells me he felt alive for the first time in a long time during the trial.
Thanks.
Has anyone here done a peripheral nerve stimulator for Occipital Neuralgia? I have a patient who has done every medical and almost every interventional option for his occipital neuralgia as well as seen tons of academic headache specialists. Nothing has worked. The only thing that has worked are Occipital nerve blocks at the ridge which provide temporary but profound relief (on the order of days to weeks). TON C3/4 Rhizotomies/blocks haven't worked either. So the other day I trialed a PNS stimulator and placed the leads at the bilateral occipital ridges kind of like this picture below (not my actual patient's picture).
It went very well. The patient had >95% relief for one week of the trial and tells me he still feels like he has some residual benefit from the trial. He was so happy. He was in tears at the follow up post op. He is really looking forward to the implant.
The problem is the company I'm using has a small IPG that I have to figure out where to put and how to tunnel it. I have several concerns and because of these concerns I may refer out or just refer to a neurosurgeon who does this but he puts the stimulator at C2 (NOT where I trialed and had major success), or maybe send to surgery for decompression.
1. I've never done one of these but it seemed easy enough to trial. I am a little concerned about the implant because I don't know a good place to place the IPG (albiet being tiny and thing. It is with mainly with this company because this is the only one my ASC approved). I am concerned about lead migration because its in the neck- an area with so much mobility.
2. It is technically considered "off-label" use of the device and I have never done one before. I don't really know anyone in my area who does much of this. I am concerned that in the event something goes wrong both of those situations can be used against me. I would like to see one being done but I don't know anyone else near me that does this.
3. The skin near the occipital ridge and the superior neck does not have much fat and so I think tunneling might be difficult.
4. Should I just NOT do this with this company and wait till my ASC approves the PNS company that does not have an IPG to tunnel to (Like StimWave)?
My main two concerns are IPG placement/tunneling as well as the technical off label use.
I really want this to work out for this patient because he is desperate has been dealing with this since being a teenager and he tells me he felt alive for the first time in a long time during the trial.
Thanks.
