- Joined
- Jul 6, 2004
- Messages
- 1,977
- Reaction score
- 563
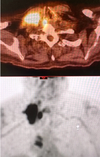
78 yo man with significant comorbidites (vasculopath, DMII with left BKA, cad, worsening dementia) has a distant history 15 years ago of treatment for dlbcl in remission now found to have growing supraclav node biopsied positive for nodular sclerosing Hodgkin's Lymphoma. Very poor chemo candidate per med onc. Asking if we can give RT alone. PET shows right cervical/supraclav nodal conglomerate and a Right IMN. What would you do here, has anyone done STLI? Just treat involved field and follow?