- Joined
- Mar 20, 2013
- Messages
- 1,920
- Reaction score
- 3,533
Mods - please move this post if most appropriate.
I do some of this type of prostate paradigm in some SBRT cases (36.25 to PTV, 40 to prostate or dominant MRI nodule).
I'm looking to integrate the FLAME regimen (77 @ 2.2 to prostate, boost MRI nodule to up to 95 Gy) and maybe I'm missing it, but I've looked at the protocol and supplements and I don't see a lot of details on margins.
This pic below is in the supplement, and the original paper has this paragraph:
"A mean dose of 77 Gy in 35 fraction of 2.2 Gy is prescribed to the entire prostate gland [33,34]. The dose in the part of the PTV overlapping the rectum and bladder is limited to keep the risk of severe gastrointestinal and genitourinary toxicity acceptable....
The precise execution of the radiotherapy treatment can differ in each participation center, but the treatment will always meet the above mentioned criteria."
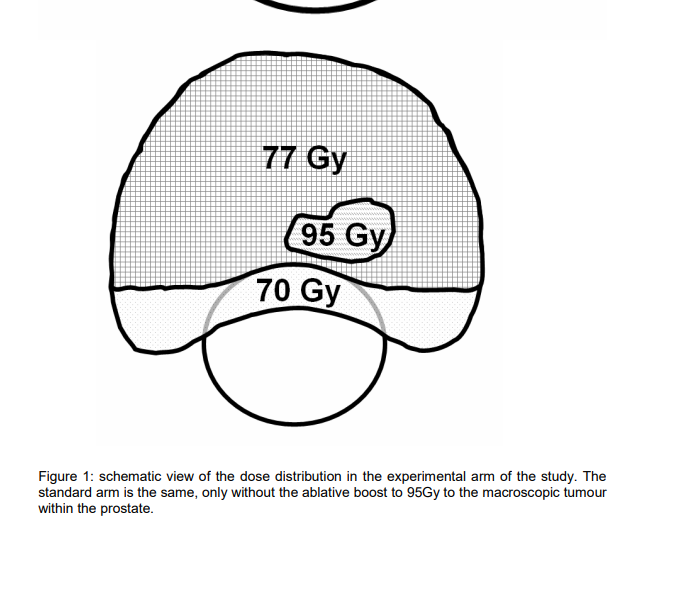
Maybe the european trials are more pragmatic, because I'm just so used to the NRG trials literally saying X mm to this margin, X mm to that margin, etc. Looks like a more classic "PTV" ?maybe prostate plus 4 mm posterior, 6-7 mm circumferential ? would get 70 Gy, the prostate should get 77 Gy, then boost the nodule to 95 Gy.
This pic is helpful, but was hoping for any tips you all have if you've been integrating this treatment into some options.
For me personally, if I have a younger patient with a clear MRI dominant area with biopsy mapping congruent (ie the high grade disease is on biopsy congruent with MRI location) I'm ready to start offering this.
I do some of this type of prostate paradigm in some SBRT cases (36.25 to PTV, 40 to prostate or dominant MRI nodule).
I'm looking to integrate the FLAME regimen (77 @ 2.2 to prostate, boost MRI nodule to up to 95 Gy) and maybe I'm missing it, but I've looked at the protocol and supplements and I don't see a lot of details on margins.
This pic below is in the supplement, and the original paper has this paragraph:
"A mean dose of 77 Gy in 35 fraction of 2.2 Gy is prescribed to the entire prostate gland [33,34]. The dose in the part of the PTV overlapping the rectum and bladder is limited to keep the risk of severe gastrointestinal and genitourinary toxicity acceptable....
The precise execution of the radiotherapy treatment can differ in each participation center, but the treatment will always meet the above mentioned criteria."
Maybe the european trials are more pragmatic, because I'm just so used to the NRG trials literally saying X mm to this margin, X mm to that margin, etc. Looks like a more classic "PTV" ?maybe prostate plus 4 mm posterior, 6-7 mm circumferential ? would get 70 Gy, the prostate should get 77 Gy, then boost the nodule to 95 Gy.
This pic is helpful, but was hoping for any tips you all have if you've been integrating this treatment into some options.
For me personally, if I have a younger patient with a clear MRI dominant area with biopsy mapping congruent (ie the high grade disease is on biopsy congruent with MRI location) I'm ready to start offering this.
