what's up?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
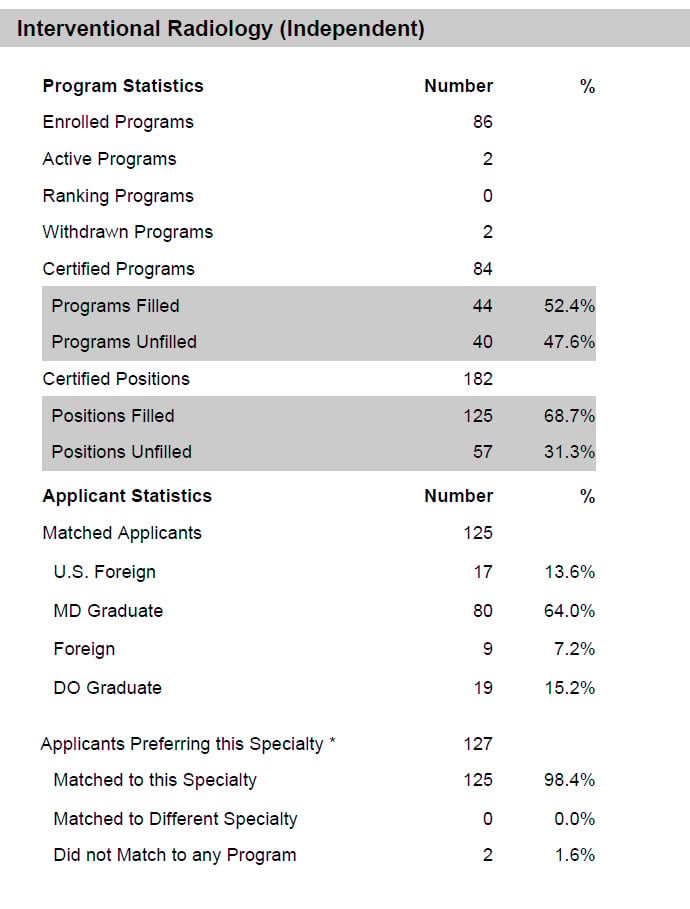
Wow--in 2022 Match, 50% of Independent IR programs go unfilled, 30% open positions
- Thread starter 5777
- Start date
- Joined
- Mar 28, 2018
- Messages
- 401
- Reaction score
- 971
Just my own personal opinion, but I believe the internet way overhyped IR as a specialty. I went into a rotation in IR fully expecting it to be some crazy "wild west" of medicine as reddit/SDN describes it. And I'm sure some procedures, on some days of the month, are like that. But the majority of it was pretty mundane procedures, with terrible hours/call schedule (at least where I rotated at). So you give up a lot of the cushiness of DR to be able to do procedures that are overwhelmingly not that exciting, and the pay, while good, is basically comparable to DR from what I can see. I don't get the hype, personally.
- Joined
- Oct 6, 2018
- Messages
- 327
- Reaction score
- 442
People interested in IR need to be very honest with themselves about what it is and what it isn’t. Most graduates will go into PP which is not interested in establishing a clinical service line, and instead cover the hospitalist gruntwork nobody else wants to do. Paras, biopsies, lines, piccs. Because of that you won’t really feel like the image-guided surgeon you sold yourself on. You could expand a service line by getting clinic time to establish practice, but you’d do so at the expense of your pay as even a high productivity clinic of well paying-high end procedures would only get you back up to speed with your diagnostic colleagues who didn’t have to establish practice in the first place.
However, it can be satisfying to people who enjoy imaging but hate how distanced they feel from seeing the consequences of what they do. You do perform high end procedures, but for the most part they are all emergent or low paying (bleeds, traumas, G / neph tubes, or dialysis access) because all the elective, endovascular, high paying stuff is spoken for by VS and IC in most places, again because they have clinic and you don’t. However, VS and IC both have nightmarish call worse than IR most of the time, so maybe it’s worth it if you want to do some endovascular. It also permits you variety in the day in PP if you want to get out of the reading room a few days a week.
The higher pay in the traditional PP model is real, but is due to the worse call schedule you’re mandated to have. A similar call schedule in DR would net you the same salary. That being said, if you’re partner in a PP and you’ve become very skilled in another specialty, you can back off in the right practice setting and let the younger folks do it. Lots of IR trained people do zero IR.
All that being said, IR is like the imaging equivalent of endovascular medicine. IC is the IM equivalent, VS is the surgical equivalent. They all cover a critical service line, they are all (for various reasons) well paid, and they all attract high-energy people who want to feel like they’re using their hands to save lives. Because they all do. What they do during the rest of the day is dependent on their primary specialty - in IR its reading imaging, in IC its medicine and cardiology (and maybe also reading imaging), in VS its GS.
However, it can be satisfying to people who enjoy imaging but hate how distanced they feel from seeing the consequences of what they do. You do perform high end procedures, but for the most part they are all emergent or low paying (bleeds, traumas, G / neph tubes, or dialysis access) because all the elective, endovascular, high paying stuff is spoken for by VS and IC in most places, again because they have clinic and you don’t. However, VS and IC both have nightmarish call worse than IR most of the time, so maybe it’s worth it if you want to do some endovascular. It also permits you variety in the day in PP if you want to get out of the reading room a few days a week.
The higher pay in the traditional PP model is real, but is due to the worse call schedule you’re mandated to have. A similar call schedule in DR would net you the same salary. That being said, if you’re partner in a PP and you’ve become very skilled in another specialty, you can back off in the right practice setting and let the younger folks do it. Lots of IR trained people do zero IR.
All that being said, IR is like the imaging equivalent of endovascular medicine. IC is the IM equivalent, VS is the surgical equivalent. They all cover a critical service line, they are all (for various reasons) well paid, and they all attract high-energy people who want to feel like they’re using their hands to save lives. Because they all do. What they do during the rest of the day is dependent on their primary specialty - in IR its reading imaging, in IC its medicine and cardiology (and maybe also reading imaging), in VS its GS.
Last edited:
- Joined
- Dec 1, 2016
- Messages
- 592
- Reaction score
- 1,081
Not at all surprised that people are not willing to two years of a grueling IR fellowship rather the 1 under the prior system.
- Joined
- Oct 6, 2018
- Messages
- 327
- Reaction score
- 442
Independent can mean 1 year after ESIR. Doesn’t have to be 2.Not at all surprised that people are not willing to two years of a grueling IR fellowship rather the 1 under the prior system.
- Joined
- Mar 12, 2019
- Messages
- 54
- Reaction score
- 25
What programs are unfilled?
- Joined
- Apr 2, 2013
- Messages
- 288
- Reaction score
- 375
Not sure if this explains the entirety of the low match rate, but number of IR applications has generally had an inverse correlation with the radiology job market. When the radiology job market is terrible, more applicants choose IR as it makes them more marketable for the many hospitals that need on-site coverage. When the job market is great as is currently, those people who would have considered IR in part for job market reasons no longer have that as a factor pushing them towards IR, when they see that they can easily get hired as a diagnostic radiology and do at least part time teleradiology with much more geographic flexibility, which you can't do with IR.
- Joined
- Sep 9, 2013
- Messages
- 111
- Reaction score
- 132
Where can we find this data? Thanks!
- Joined
- Mar 4, 2017
- Messages
- 286
- Reaction score
- 626
NRMP posts this information: link
The report for positions starting 2023 has not yet been created. But the information 5777 posted was released on Fellowship Match day to institutions and programs, and should be available in the next report.
I've attached the page about IR from the latest report for IR that is available from NRMP that includes data up to positions starting in 2022. You can see that by all metrics, the independent IR stats have indeed fallen off a cliff. The other areas (Breast, MSK, Neuroradiology) did collectively a bit better than last year (Breast had 18.0% unfilled positions this year compared to 21.9% last year, MSK had 20.8% unfilled positions this year compared to 19.4% last year, Neuroradiology had 14.4% unfilled positions this year compared to 17.5% last year).
So, it isn't just the excellent current job market. But there is a very good reason, and it isn't that people have soured on IR so much as that there is a limit to how many people are interested in IR.
Now that IR grabs very interested people out of medical school into integrated programs, there are fewer remaining folks in DR who are super interested in IR--some, but not nearly as many. There's a fixed limit to the number of people who have radiology interests who want to do IR, and now the sum total of IR training spots out there way exceeds the number.
If you go back, to the integrated residency information from NRMP, there were 118 integrated IR spots filled in the 2017 Residency Match (27 of 29 available categorical, 91 of 95 available advanced)--after doing an internship from 2017-2018, that cohort are starting their final year of IR in July 2022, and will graduate in 2023. They are joined by the 141 Independent IR residents who matched into an independent program in June 2021, graduating from their DR program this June and starting the IR year in July 2022, and finishing their IR training in June 2023. So, in June 2023, there will be 259 IR graduates (assuming everyone stayed in the program and graduates).
There were 133 integrated IR spots filled in the 2018 Residency Match (35 of 35 available categorical, 98 of 98 available advanced). These trainees will finish IR in June 2024, and will be joined by the 125 Independent IR residents who just matched in June 2022. So, in June 2024, there will be 258 IR graduates (again, assumes everyone stays in the program and graduates). Really, no meaningful change in the number (258 vs 259).
What did change was the number of positions, because there were 182 independent spots along with the original 133 integrated spots, for a total of 315. Last year, there were 166 independent spots along with the original 124 integrated spots, for a total of 292. So an increase by 7.9%.
A look forward from past Residency Match shows what is coming down the pike. For Integrated programs, there were 150 spots filled from 150 available in 2019, 148 filled from 156 available in 2020, 155 filled from 162 available in 2021, and 168 filled from 168 available in 2022.
If the number of individuals interested in IR is "fixed" at around 260 people, then fewer independent spots will be filled going forward, since there are more individuals committed in integrated spots.
It may turn out that programs will "turn off" their independent IR programs or decrease those spots now that they have integrated IR programs and spots. I'm sure some of that will happen.
But the thing about these training spots is that they are like drugs to programs--once they have them and have secured institutional funding support for them, they suddenly "need" all of these trainees on service and are disinclined to give them up.
The implication being that if you aren't sure about IR vs DR as a medical student, your absolute best bet is to get the best DR spot you can get (preferably at a place that has ESIR possibility, which won't be as competitive because your DR cohort won't have as many people who are actually interested in IR). As a DR resident who performs well and who makes a reasonable effort to make IR connections once you decide that's your route, you won't have difficulty going into IR later, as I predict there are going to be a lot of independent spots that stay open for a while even if they go unfilled.
The report for positions starting 2023 has not yet been created. But the information 5777 posted was released on Fellowship Match day to institutions and programs, and should be available in the next report.
I've attached the page about IR from the latest report for IR that is available from NRMP that includes data up to positions starting in 2022. You can see that by all metrics, the independent IR stats have indeed fallen off a cliff. The other areas (Breast, MSK, Neuroradiology) did collectively a bit better than last year (Breast had 18.0% unfilled positions this year compared to 21.9% last year, MSK had 20.8% unfilled positions this year compared to 19.4% last year, Neuroradiology had 14.4% unfilled positions this year compared to 17.5% last year).
So, it isn't just the excellent current job market. But there is a very good reason, and it isn't that people have soured on IR so much as that there is a limit to how many people are interested in IR.
Now that IR grabs very interested people out of medical school into integrated programs, there are fewer remaining folks in DR who are super interested in IR--some, but not nearly as many. There's a fixed limit to the number of people who have radiology interests who want to do IR, and now the sum total of IR training spots out there way exceeds the number.
If you go back, to the integrated residency information from NRMP, there were 118 integrated IR spots filled in the 2017 Residency Match (27 of 29 available categorical, 91 of 95 available advanced)--after doing an internship from 2017-2018, that cohort are starting their final year of IR in July 2022, and will graduate in 2023. They are joined by the 141 Independent IR residents who matched into an independent program in June 2021, graduating from their DR program this June and starting the IR year in July 2022, and finishing their IR training in June 2023. So, in June 2023, there will be 259 IR graduates (assuming everyone stayed in the program and graduates).
There were 133 integrated IR spots filled in the 2018 Residency Match (35 of 35 available categorical, 98 of 98 available advanced). These trainees will finish IR in June 2024, and will be joined by the 125 Independent IR residents who just matched in June 2022. So, in June 2024, there will be 258 IR graduates (again, assumes everyone stays in the program and graduates). Really, no meaningful change in the number (258 vs 259).
What did change was the number of positions, because there were 182 independent spots along with the original 133 integrated spots, for a total of 315. Last year, there were 166 independent spots along with the original 124 integrated spots, for a total of 292. So an increase by 7.9%.
A look forward from past Residency Match shows what is coming down the pike. For Integrated programs, there were 150 spots filled from 150 available in 2019, 148 filled from 156 available in 2020, 155 filled from 162 available in 2021, and 168 filled from 168 available in 2022.
If the number of individuals interested in IR is "fixed" at around 260 people, then fewer independent spots will be filled going forward, since there are more individuals committed in integrated spots.
It may turn out that programs will "turn off" their independent IR programs or decrease those spots now that they have integrated IR programs and spots. I'm sure some of that will happen.
But the thing about these training spots is that they are like drugs to programs--once they have them and have secured institutional funding support for them, they suddenly "need" all of these trainees on service and are disinclined to give them up.
The implication being that if you aren't sure about IR vs DR as a medical student, your absolute best bet is to get the best DR spot you can get (preferably at a place that has ESIR possibility, which won't be as competitive because your DR cohort won't have as many people who are actually interested in IR). As a DR resident who performs well and who makes a reasonable effort to make IR connections once you decide that's your route, you won't have difficulty going into IR later, as I predict there are going to be a lot of independent spots that stay open for a while even if they go unfilled.
Attachments
Last edited:
- Joined
- Mar 4, 2017
- Messages
- 286
- Reaction score
- 626
What's really interesting is to consider what impact this whole "Integrated IR" system has had.
The 2017 Specialties Match was the apex of the previous "IR Fellowship" paradigm--there were 252 IR spots available for applicants who would complete their IR training in 2019. Of these spots, 97.2% were filled, for a total of 245 IR graduates. Not much different than the 260 graduate number we might be stuck at.
So it seems to me that the underlying idea that was the foundational belief of the IR academics that pushed so hard for this "separate IR" system is suspect. The idea was that if they could just get into the heads of potential trainees by having them choose IR during medical school instead of after being in radiology residency there would be an explosion of new interest in IR, that more people would want to train in IR. IR would get their fraction of the people who were going into Radiology, as well as pull in people who would have instead gone into some surgical field out of medical school.
In so doing, the idea was that the radiology-based procedural needs of every patient at every health facility in the country could be addressed by an IR rad (since there would be so many), and that the people going into IR would be "better".
I beg to differ. We would have been far far better off keeping IR as a fellowship, giving trainees a chance to really choose IR based on experience as a radiology resident. The individuals who built IR into what it is today were all DR residents first--that system worked.
The 2017 Specialties Match was the apex of the previous "IR Fellowship" paradigm--there were 252 IR spots available for applicants who would complete their IR training in 2019. Of these spots, 97.2% were filled, for a total of 245 IR graduates. Not much different than the 260 graduate number we might be stuck at.
So it seems to me that the underlying idea that was the foundational belief of the IR academics that pushed so hard for this "separate IR" system is suspect. The idea was that if they could just get into the heads of potential trainees by having them choose IR during medical school instead of after being in radiology residency there would be an explosion of new interest in IR, that more people would want to train in IR. IR would get their fraction of the people who were going into Radiology, as well as pull in people who would have instead gone into some surgical field out of medical school.
In so doing, the idea was that the radiology-based procedural needs of every patient at every health facility in the country could be addressed by an IR rad (since there would be so many), and that the people going into IR would be "better".
I beg to differ. We would have been far far better off keeping IR as a fellowship, giving trainees a chance to really choose IR based on experience as a radiology resident. The individuals who built IR into what it is today were all DR residents first--that system worked.
- Joined
- Oct 6, 2018
- Messages
- 327
- Reaction score
- 442
IR is stuck between a rock and a hard place. It may be a field worth pursuing if their diagnostic counterparts would give them clinic time in the private practice setting to recruit more interesting procedures to their scope.What's really interesting is to consider what impact this whole "Integrated IR" system has had.
The 2017 Specialties Match was the apex of the previous "IR Fellowship" paradigm--there were 252 IR spots available for applicants who would complete their IR training in 2019. Of these spots, 97.2% were filled, for a total of 245 IR graduates. Not much different than the 260 graduate number we might be stuck at.
So it seems to me that the underlying idea that was the foundational belief of the IR academics that pushed so hard for this "separate IR" system is suspect. The idea was that if they could just get into the heads of potential trainees by having them choose IR during medical school instead of after being in radiology residency there would be an explosion of new interest in IR, that more people would want to train in IR. IR would get their fraction of the people who were going into Radiology, as well as pull in people who would have instead gone into some surgical field out of medical school.
In so doing, the idea was that the radiology-based procedural needs of every patient at every health facility in the country could be addressed by an IR rad (since there would be so many), and that the people going into IR would be "better".
I beg to differ. We would have been far far better off keeping IR as a fellowship, giving trainees a chance to really choose IR based on experience as a radiology resident. The individuals who built IR into what it is today were all DR residents first--that system worked.
But the diagnostic guys don’t, and the interventional guys often don’t want to do it on their own because they’d rather have the higher salary straight out the gate than deal with building a practice from the ground up with no referral patterns to begin with.
- Joined
- Aug 19, 2013
- Messages
- 16
- Reaction score
- 10
Practice building is tough, time consuming, and as you said, often not well regarded or compensated in the early years.
It is also not something that all, or many IR programs train you well in. Yes, the clinical model is large and growing, but most places that practice the clinical model are already established with strong referral bases. You are never involved in building the practice as a trainee so you don't have these skills.
I imagine upon leaving into a real job and given the option of taking a job with light IR that requires no extra dedication to creating a service and one where you would have to put in a lot of effort to create one, it just makes more sense to go the path of least resistance.
One interesting thing I have found is the preponderance of OBL type jobs that are pure IR and do allow and encourage this pathway, which is a good option for those interested. Unfortunately, nearly all of these types of jobs are devoid of any diagnostic responsibilities which I think a sizable chunk of people would want at least some of. I guess there's always the addition of moonlighting/locums.
It is also not something that all, or many IR programs train you well in. Yes, the clinical model is large and growing, but most places that practice the clinical model are already established with strong referral bases. You are never involved in building the practice as a trainee so you don't have these skills.
I imagine upon leaving into a real job and given the option of taking a job with light IR that requires no extra dedication to creating a service and one where you would have to put in a lot of effort to create one, it just makes more sense to go the path of least resistance.
One interesting thing I have found is the preponderance of OBL type jobs that are pure IR and do allow and encourage this pathway, which is a good option for those interested. Unfortunately, nearly all of these types of jobs are devoid of any diagnostic responsibilities which I think a sizable chunk of people would want at least some of. I guess there's always the addition of moonlighting/locums.
There is becoming a noted difference between integrated residents and ESIR residents applying for independent 1 or 2 year spots. The students applying into integrated are much more surgical in nature and in general want a patient facing specialty. They are often doing multiple surgical rotations during their 4th year, vascular surgery, busy VIR sub internships .
However, there are many who did not really get a good feel for what VIR is during medical school (they did very little IR during medical school and when on IR were more of an observorship (9 to 5) scrubbing in cases not spending time in clinic or staying late or covering call. Busy sub internships and surgical rotations such as vascular surgery give one a much better understanding of what VIR is becoming.
There are some who go into IR residency and realize they enjoy imaging quite a bit and do not like the unpredictable nature of VIR or dealing with complications etc, those will consider procedural subspecialties (mammography,MSK, body , neuro etc) and they may drop out of the IR residency. In those programs they are often able to find an internal transfer from DR to IR.
The various programs decided to increase their complement of 1 and 2 year independent residents as it is easier to pay for that as opposed to funding a 6 year integrated resident.
It will likely level out, but the modern day VIR will certainly have to go out and build their infrastructure and clinical practice which is a lot of work
see post
 linemonkeymd.com
linemonkeymd.com
Will be a great deal of paradigm shift as VIR start to market more and more to primary care and patients themselves for
Fibroids , BPH, knee pain, back pain, osteoporotic compression fractures, PAD, DVT/ PE etc. For the motivated individual times have never been better, but it is a lot of work.
However, there are many who did not really get a good feel for what VIR is during medical school (they did very little IR during medical school and when on IR were more of an observorship (9 to 5) scrubbing in cases not spending time in clinic or staying late or covering call. Busy sub internships and surgical rotations such as vascular surgery give one a much better understanding of what VIR is becoming.
There are some who go into IR residency and realize they enjoy imaging quite a bit and do not like the unpredictable nature of VIR or dealing with complications etc, those will consider procedural subspecialties (mammography,MSK, body , neuro etc) and they may drop out of the IR residency. In those programs they are often able to find an internal transfer from DR to IR.
The various programs decided to increase their complement of 1 and 2 year independent residents as it is easier to pay for that as opposed to funding a 6 year integrated resident.
It will likely level out, but the modern day VIR will certainly have to go out and build their infrastructure and clinical practice which is a lot of work
see post
The Founder Mentality – Line Monkey MD
 linemonkeymd.com
linemonkeymd.com
Will be a great deal of paradigm shift as VIR start to market more and more to primary care and patients themselves for
Fibroids , BPH, knee pain, back pain, osteoporotic compression fractures, PAD, DVT/ PE etc. For the motivated individual times have never been better, but it is a lot of work.
- Joined
- Sep 2, 2011
- Messages
- 106
- Reaction score
- 68
I think this is a pretty hot take, lots of issues with this. Surgically minded students usually end up going into surgery, that's usually how that goes. If anything there's a pretty sizeable pool of people who filter over to DR at some point during surgery or after not matching into a subspecialty, these folks are much more surgical than your typical direct to IR applicant, having been willing to live that life, and in many cases having experienced that for at least a couple years.There is becoming a noted difference between integrated residents and ESIR residents applying for independent 1 or 2 year spots. The students applying into integrated are much more surgical in nature and in general want a patient facing specialty. They are often doing multiple surgical rotations during their 4th year, vascular surgery, busy VIR sub internships .
However, there are many who did not really get a good feel for what VIR is during medical school (they did very little IR during medical school and when on IR were more of an observorship (9 to 5) scrubbing in cases not spending time in clinic or staying late or covering call. Busy sub internships and surgical rotations such as vascular surgery give one a much better understanding of what VIR is becoming.
There are some who go into IR residency and realize they enjoy imaging quite a bit and do not like the unpredictable nature of VIR or dealing with complications etc, those will consider procedural subspecialties (mammography,MSK, body , neuro etc) and they may drop out of the IR residency. In those programs they are often able to find an internal transfer from DR to IR.
The various programs decided to increase their complement of 1 and 2 year independent residents as it is easier to pay for that as opposed to funding a 6 year integrated resident.
It will likely level out, but the modern day VIR will certainly have to go out and build their infrastructure and clinical practice which is a lot of work
see post
The Founder Mentality – Line Monkey MD
linemonkeymd.com
Will be a great deal of paradigm shift as VIR start to market more and more to primary care and patients themselves for
Fibroids , BPH, knee pain, back pain, osteoporotic compression fractures, PAD, DVT/ PE etc. For the motivated individual times have never been better, but it is a lot of work.
I think more of the direct to IR applicants fall within that second category you mentioned, and usually it ends up being some subconscious combination of having really high scores and wanting something prestigious and procedurally oriented (and IR is marketed to med students as being VERY prestigious based on the competitiveness of the integrated pathway), but also genuinely NOT wanting to commit to the surgery lifestyle and wanting the DR backup.
Then they get into training and realize that it's not at all like what was advertised, and you basically either get to be a dumping ground for the hospital while wearing the golden handcuffs of DR (with added radiation exposure and call requirements for nearly the same money in some practices), or you have to literally fight tooth and nail for your cases, clinic, open an OBL etc. All of this is contradictory to the decision they made as a med student, influenced at least on a subconscious level by perceived prestige and lifestyle. And it's not like they have some really special integrated training to do all that, they're still doing 3 years of DR +2 years of IR no matter how you slice it. An extra ICU rotation here or there isn't doing all that much, and in fact they may even end up with less total years of training vs a DR with 1+4+2.
In contrast, many of the residents who apply to IR from DR have had a much deeper experience with IR, they've been in a much more involved role on the service, they've taken call, they've seen the lives their attendings live and the frictions between IR/DR and IR/other specialties, and they at least know what they're getting into.
Last edited:
- Joined
- Oct 6, 2018
- Messages
- 327
- Reaction score
- 442
I think this is a pretty hot take, lots of issues with this. Surgically minded students usually end up going into surgery, that's usually how that goes. If anything there's a pretty sizeable pool of people who filter over to DR at some point during surgery or after not matching into a subspecialty, these folks are much more surgical than your typical direct to IR applicant, having been willing to live that life, and in many cases having experienced that for at least a couple years.
I think more of the direct to IR applicants fall within that second category you mentioned, and usually it ends up being some subconscious combination of having really high scores and wanting something prestigious and procedurally oriented (and IR is marketed to med students as being VERY prestigious based on the competitiveness of the integrated pathway), but also genuinely NOT wanting to commit to the surgery lifestyle and wanting the DR backup.
Then they get into training and realize that it's not at all like what was advertised, and you basically either get to be a dumping ground for the hospital while wearing the golden handcuffs of DR (with added radiation exposure and call requirements for nearly the same money in some practices), or you have to literally fight tooth and nail for your cases, clinic, open an OBL etc. All of this is contradictory to the decision they made as a med student, influenced at least on a subconscious level by perceived prestige and lifestyle. And it's not like they have some really special integrated training to do all that, they're still doing 3 years of DR +2 years of IR no matter how you slice it. An extra ICU rotation here or there isn't doing all that much, and in fact they may even end up with less total years of training vs a DR with 1+4+2.
In contrast, many of the residents who apply to IR from DR have had a much deeper experience with IR, they've been in a much more involved role on the service, they've taken call, they've seen the lives their attendings live and the frictions between IR/DR and IR/other specialties, and they at least know what they're getting into.
Every surgeon has to fight tooth and nail to establish practice, IR is no exception.
However now with the job market as hot as it is practices may not have to be open to IR trying to establish practice. The IR will have to make sacrifices, but the DR group doesn’t have the luxury of dictating to the IR what they will do anymore.
- Joined
- Sep 2, 2011
- Messages
- 106
- Reaction score
- 68
What surgeons fight tooth and nail to establish practice? For most of them it's as easy as getting put on the call schedule and then starting to generate referrals as long as they're halfway decent and not a complete jerk to people on the phone. Some even get away with this and still do fine. They don't have nearly the same hurdles of pseudo-exclusive contracts, competition from other specialties for interventional procedures, being a "dumping ground" for other specialties undesirable procedures etc.Every surgeon has to fight tooth and nail to establish practice, IR is no exception.
However now with the job market as hot as it is practices may not have to be open to IR trying to establish practice. The IR will have to make sacrifices, but the DR group doesn’t have the luxury of dictating to the IR what they will do anymore.
Also, I have to push back on the whole "IR are surgeons, no exceptions" thing. Virtually every physician can technically be considered a physician and surgeon. But once IR starts labeling themselves as surgeons the battle is lost by default. There needs to be an emphasis on the fact that the critical skill underlying the practice of interventional radiology is radiology. Unfortunately that somehow seemed to get lost in the shuffle, and that's what has resulted in so much encroachment from other specialties. When their radiology skills aren't up to par it shows in every element of the work. We need to stand more strongly behind the fact that we are the experts at image interpretation and image guided procedures, and that expertise is based on our ability as radiologists and NOT as surgeons and that's what makes us different.
- Joined
- Oct 6, 2018
- Messages
- 327
- Reaction score
- 442
It always amuses me when IR docs who don’t give grand rounds, don’t give lunch talks, don’t spend money to advertise services then wonder why they don’t get any high end procedural referrals. An IR that successfully establishes practice doesn’t do much more work than surgeons who have to do the same thing. You can’t be a surgeon who wants to do 100% high paying elective procedures who just sits on their butt and wait on a referral pattern to build by existing. Several family members of mine are surgeons and they will tell you the same thing. If you work in a market where one service line is saturated, yes it’s very tough without senior practice members throwing you a bone, that’s true for surgeons too. If you work for a practice that neglected and atrophied it’s service line (very common) and made no effort to maintain a referral base, and whine when they lost it, yes you have an uphill battle.What surgeons fight tooth and nail to establish practice? For most of them it's as easy as getting put on the call schedule and then starting to generate referrals as long as they're halfway decent and not a complete jerk to people on the phone. Some even get away with this and still do fine. They don't have nearly the same hurdles of pseudo-exclusive contracts, competition from other specialties for interventional procedures, being a "dumping ground" for other specialties undesirable procedures etc.
Also, I have to push back on the whole "IR are surgeons, no exceptions" thing. Virtually every physician can technically be considered a physician and surgeon. But once IR starts labeling themselves as surgeons the battle is lost by default. There needs to be an emphasis on the fact that the critical skill underlying the practice of interventional radiology is radiology. Unfortunately that somehow seemed to get lost in the shuffle, and that's what has resulted in so much encroachment from other specialties. When their radiology skills aren't up to par it shows in every element of the work. We need to stand more strongly behind the fact that we are the experts at image interpretation and image guided procedures, and that expertise is based on our ability as radiologists and NOT as surgeons and that's what makes us different.
I don’t like these pedantic battles based on what things are called - surgery vs not. If you make an effort to take care of patients before, during, and after a procedure, you can call yourself whatever you want.
Most surgical and procedural specialties have to build their referral base. Young surgeons/proceduralists often take extra call to get the foot in the door so they can build their practice. It takes time and hard work and 3 to 5 years. If you are hired by a hospital or a group you have a stipend but eventually have to collect adequate Billings. Radiology, path, anesthesia, er; hospitalists (shift workers) have more of a defined schedule and don't have to practice build as much. VIR in order to do higher end outpatient work have to really go out there and hustle to build a referral bin (outside of transplant centers/cancer centers or trauma centers where much of that work may be "handed to them")
Cardiologists are very good at cardiac imaging including echo, ct, MRI, nuclear medicine etc. They also generate level 1 evidence for what they do. Very few radiologists are competent in conventional coronary angiography or echocardiography. More and more neurologists and neurosurgeons are pretty good at stroke imaging and those who train in cerebral angiography are better at cerebral angiography imaging when compared to most graduating diagnostic radiology residents. So, I think the imaging of any organ can for the most part can be taught to and learned by most organ specialists. What sets VIR physicians apart is there diversity of diseases that they see (intervention oncology, HCC/ Renal masses, neuroendocrine, lung cancer, bone mets) ; portal hypertension (varices/ ascites/ TIPS/BRTO /Denver shunts); vertebral augmentation (spine jack/ kypho/vertebroplasty/esi/ rhizotomy); knee pain (GAE); BPH (PAE); fibroids (UAE); PAD/CLI; stroke ; carotid disease; billiary (spyglass) etc.
Cardiologists are very good at cardiac imaging including echo, ct, MRI, nuclear medicine etc. They also generate level 1 evidence for what they do. Very few radiologists are competent in conventional coronary angiography or echocardiography. More and more neurologists and neurosurgeons are pretty good at stroke imaging and those who train in cerebral angiography are better at cerebral angiography imaging when compared to most graduating diagnostic radiology residents. So, I think the imaging of any organ can for the most part can be taught to and learned by most organ specialists. What sets VIR physicians apart is there diversity of diseases that they see (intervention oncology, HCC/ Renal masses, neuroendocrine, lung cancer, bone mets) ; portal hypertension (varices/ ascites/ TIPS/BRTO /Denver shunts); vertebral augmentation (spine jack/ kypho/vertebroplasty/esi/ rhizotomy); knee pain (GAE); BPH (PAE); fibroids (UAE); PAD/CLI; stroke ; carotid disease; billiary (spyglass) etc.
- Joined
- Sep 2, 2011
- Messages
- 106
- Reaction score
- 68
This has to be a joke right? First of all this is in no way an apples to apples comparison to compare endovascular trained neurosurgeons or neurologists to an "average DR" resident with regards to cerebral angiography. The kinds of DR residents out there intending to go into NIR have clocked thousands of procedure and are absolutely competitive with these other specialties mentioned. From first hand experience, some of these other specialists start off FAR FAR behind in interventional experience and skill in NIR specifically. Yes they may catch up, particularly the few that end up in top fellowships (mostly taught by neurosurgery and radiology).More and more neurologists and neurosurgeons are pretty good at stroke imaging and those who train in cerebral angiography are better at cerebral angiography imaging when compared to most graduating diagnostic radiology residents. So, I think the imaging of any organ can for the most part can be taught to and learned by most organ specialists.
But this is the exact issue that I'm getting at. For some reason radiologists as a whole always seem willing to demean themselves and their specialty and elevate other specialties. What I'm saying is if we actually had some self respect for our role and what we bring to the table we wouldn't need to try to aspire to be another specialty entirely. If anything, it's these specialties aspiring to be like us because image guided minimally invasive interventions are the future and have been for a long time now.
Not comparing a neurointerventionalist with Interventional rads/ neuroradiologic background to a neurosurgeon or neurologist. In those cases I do agree the catheter skills and imaging skill prowess is quite high. I am talking about the graduating diagnostic radiology resident who goes on to do fellowship in nuclear/mammo/ MSK etc . The volume of cerebral angiography that the current DR residents sees and performs is very low.
