- Joined
- Jan 14, 2006
- Messages
- 11,891
- Reaction score
- 20,952
Glad they finally addressed gum. Hopefully it will save some phone calls from preop. I’ve always ignored it.

 pubs.asahq.org
pubs.asahq.org
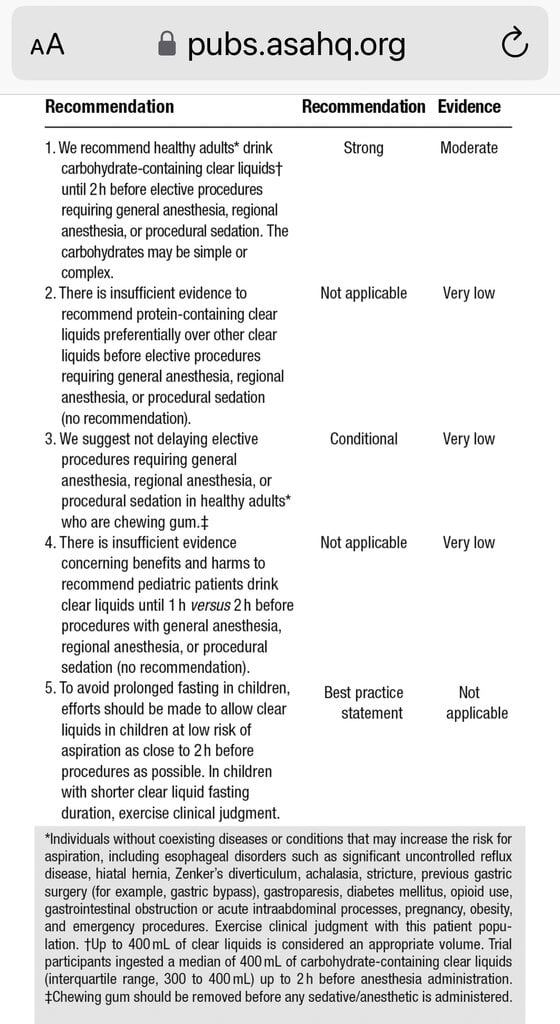

2023 American Society of Anesthesiologists Practice Guidelines for Preoperative Fasting: Carbohydrate-containing Clear Liquids with or without Protein, Chewing Gum, and Pediatric Fasting Duration—A Modular Update of the 2017 American Society of Anest
These practice guidelines are a modular update of the “Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures.” The guidance focuses on topics not addressed in the...

