What do you honestly expect a CAQ in surgery from the non-surgical board to say to an employer the person is applying to?
Huh? We are not the "non-surgical board". We are the American Board of Podiatric Medicine and we offer multiple independently-validated examinations. One of those examinations is the ABPM Certification Exam which is the recognized exam by CPME for podiatric orthopaedics and primary podiatric medicine.
Also we're all DPMs, we're not DPSs.
You are talking about passing a written test... written.
First, that's not all one must do to be eligible, explained below. Second, I'm always open to suggestions. So please, tell me how to create a psychometrically-valid, objective assessment of one's surgical knowledge or ability? We've been through this with psychometrists over-and-over.
ABPM actually used to require case documentation for its certification exam. Our external psychometrists (who are the same for many boards, BTW) told us it was impossible to make those assessment objective. And then we decided to separately evaluate them and we found that cases made little difference in the overall pass rate. Therefore, if it's a subjective measure and makes little to no difference, why do it? Except to gate keep. Furthermore, it was the biggest liability for the ABPM (and I'll argue any certifying board, because it will be why a board gets sued. They won't get sued over a validated multiple choice question.
If you want to take this one step further and say, yes, but you must evaluate someones skill, not just their knowledge, for them to do surgery. There are already skills assessments in place ... also subjective, but they are there.
1. The skills assessment in residency training (which could be improved and do you know who tried to improve it at the CPME 320 rewrite ... we did!)
2. The privileging process. Both in the initial granting of privileges and continued privileges. It is when you can have direct observation by a peer and if you have too many failures or infections, the system is supposed to re-review.
Meanwhile, in podiatry, somebody who did any bottom-of-the-barrel DPM residency could have a cert in podiatric medicine, and now they could have a certificate in podiatric surgery (from the medicine board!) if they are minimally competent in written test-taking? They could do all this without ever having done a single OR surgery themselves - and maybe the never will... yet they are CAQ for surgery forever if they will pay their dues. Does that make any sense to you?? Someone who has never done a toe amp or a soft tissue mass can be lifetime cert for surgery? It does not make any sense to me.
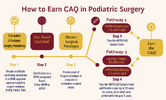
Totally false. The CAQ is not a demonstration of minimal competence. That is a licensing exam. You have to be first licensed and board certified
before you sit for a CAQ. You've already met minimal competence.
And you have to have surgical privileges in addition to primary board certification in order to be eligible to sit for the CAQ in PS. You must continue to demonstrate those surgical privileges. If you lose your privileges, your CAQ in PS is revoked.
And you like to point out the Pathway 1 which is only for those who finished their residency within the past 3 years. Already we've established in many posts that everyone thinks you're competent to do surgery then, the other board, hospitals, governments, peers, etc. Because if you weren't competent, why would you get granted surgical privileges? Do you think you get privileges to independently "practice" on people and complete your Jedi training? The real answer is that you have
proximity to your training and the volume of cases you were required to do by CPME is considered sufficient. Even the CMS requirements which state that clinical privileges must be based on a provider's
education, training, and experience, is further clarified as
current experience. That is defined as the last 24 months of surgical activity.
We recognize that in Pathway 1. (We chose 3 years instead of 2 based on the timing of the CAQ exams in March and that is not a full year from when you finish residency in July, so we thought is was more fair to be 3 years - which is really 2 years and 8 months).
In Pathway 2, if you are more than 3 years out, you must demonstrate your
current experience by a case documentation process. How many cases should you submit? You tell me? It doesn't mean those are the only cases you've performed. It's a representative sample of your surgical work in a diversity of categories. How many is fair to demonstrate that? Please, and I'm not being sarcastic, tell me how many is a representative sample and is fair?