Is anyone not recommending XRT for rectal cancer staged with MRI that is T3 or N1? For instance if it is a T3 N1 tumor but it is seen to to have a "safe" resection plane and not have any on the negative predictors (i.e. EMVI , tumors less than 4.0 cm from the anal verge, and anterior tumors).
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Mercury II
- Thread starter xrt123
- Start date
if it is a high T3N0, some large volume centers like MSKCC may argue to omit radiation. I cant see anyone suggesting leaving it out for N1, although there is an intergroup study randomizing neoadjuvant xrt vs folfox presently.
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
No. It doesn't even seem like the study has finished and reported results yet....Is anyone not recommending XRT for rectal cancer staged with MRI that is T3 or N1? For instance if it is a T3 N1 tumor but it is seen to to have a "safe" resection plane and not have any on the negative predictors (i.e. EMVI , tumors less than 4.0 cm from the anal verge, and anterior tumors).
Low Rectal Cancer Study (MERCURY II) - Full Text View - ClinicalTrials.gov
Sent from my SAMSUNG-SM-N910A using SDN mobile
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
Is there a protocol? Never heard of this study. I don't see where they're suggesting cutting out neoadjuvant CRT.
Wouldn't omit RT, definitely not in cN1 on imaging.
Wouldn't omit RT, definitely not in cN1 on imaging.
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
Mri obtained after chemo/xrt before surgery?I know published data looks pretty good, but in practice I've been stunned how inaccurate preop MRI was for rectal cancer. cT3N1 = pT2 so often
No, at initial diagnosis.
Mri obtained after chemo/xrt before surgery?
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
So then neoadj treatment could have caused that downstagingNo, at initial diagnosis.
Sent from my SAMSUNG-SM-N910A using SDN mobile
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
I know published data looks pretty good, but in practice I've been stunned how inaccurate preop MRI was for rectal cancer. cT3N1 = pT2 so often
Do you mean cT3N1 = ypT2 after neoadjuvant CRT?
No, at my hospital we have patients see all modalities ("colorectal clinic") before any treatment. Some had "staging MRI" upfront. Multiple cases went to straight surgery despite locally advanced MRI read. A common pathological finding was stage I disease.
I think for a meaningful rectal MRI you need: 1) high Tesla magnet; 2) endorectal coil; 3) dedicated radiologist.
Similar caveats probably apply for EUS staging.
Therefore, in a community setting, preop XRT is often overkill.
I think for a meaningful rectal MRI you need: 1) high Tesla magnet; 2) endorectal coil; 3) dedicated radiologist.
Similar caveats probably apply for EUS staging.
Therefore, in a community setting, preop XRT is often overkill.
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
Are they having any adjunctive staging imaging? PET/CT to evaluate PET-avidity of enlarged lymph nodes picked up on MRI? Interesting to see cN1 = pN0 in some cases. I wonder what the percentage of that in rectal cancer is. I'd consider writing that up if I was you, would be an interesting case series IMO.
Personally, I favor ERUS more than MRI for most accurate T-staging.
Personally, I favor ERUS more than MRI for most accurate T-staging.
- Joined
- Mar 20, 2013
- Messages
- 1,920
- Reaction score
- 3,534
At our center we have an MRI body guy that is the only one that reads all the MRI pelvis/rectal cancer cases.
One surgical oncologist (kind of the local leader in rectal cancer) that is particularly interested in this did about 20-30 cases that all had both EUS and MRI (with the MRI pelvis radiologist looking at the scans with the surgeon together for each case) and there was near perfect correlation between findings there (as in EUS and MRI seemed equivocal and had pretty good rad to path T staging correlation for the T2's) to the point where our surg oncs quit sending for EUS and like the MRI better for whatever reason. By the time I see the patient they've already had MRI or rarely EUS.
For high T3N0 cases one of our surg oncs feels comfortable with no pre-op XRT. Only really for ~8-10 cm and up though. Data there is compelling that it's probably OK as long as you sample at least 10 nodes with more limited benefit for preop XRT. Our other surg oncs push hard for preop XRT on all T3's.
You're dealing with an area where a good TME is probably good enough for a lot of patients...but the death/issues with a local relapse is absolutely awful and pre-op rectal cancer XRT really isn't too toxic most of the time...so at our multidisciplinary clinic/tumor boards, most push for what is probably over treatment on borderline cases with pre op XRT.
One surgical oncologist (kind of the local leader in rectal cancer) that is particularly interested in this did about 20-30 cases that all had both EUS and MRI (with the MRI pelvis radiologist looking at the scans with the surgeon together for each case) and there was near perfect correlation between findings there (as in EUS and MRI seemed equivocal and had pretty good rad to path T staging correlation for the T2's) to the point where our surg oncs quit sending for EUS and like the MRI better for whatever reason. By the time I see the patient they've already had MRI or rarely EUS.
For high T3N0 cases one of our surg oncs feels comfortable with no pre-op XRT. Only really for ~8-10 cm and up though. Data there is compelling that it's probably OK as long as you sample at least 10 nodes with more limited benefit for preop XRT. Our other surg oncs push hard for preop XRT on all T3's.
You're dealing with an area where a good TME is probably good enough for a lot of patients...but the death/issues with a local relapse is absolutely awful and pre-op rectal cancer XRT really isn't too toxic most of the time...so at our multidisciplinary clinic/tumor boards, most push for what is probably over treatment on borderline cases with pre op XRT.
"No. It doesn't even seem like the study has finished and reported results yet...."
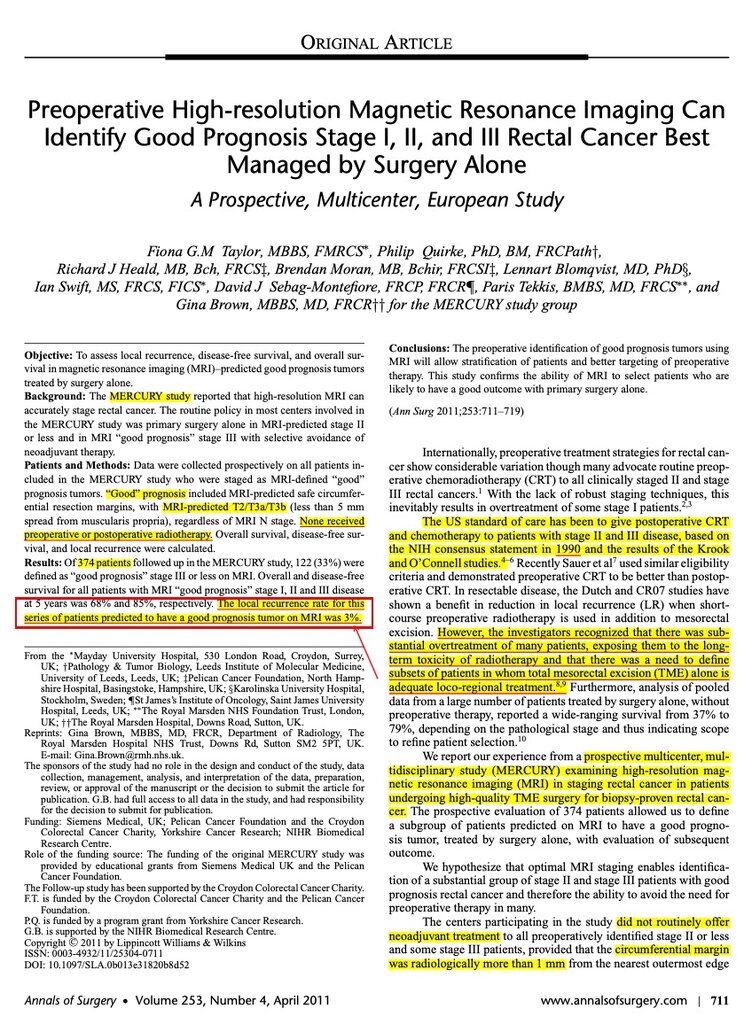
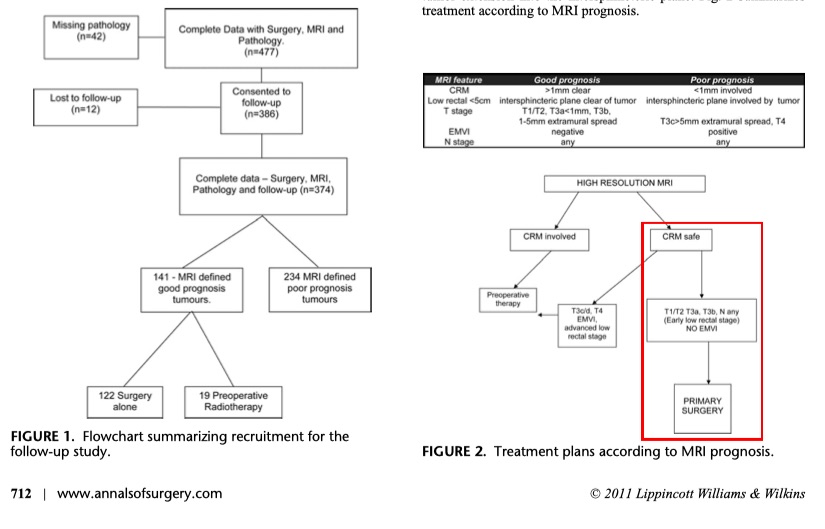
There is a publication in the Annals of Surgery (not sure if more are pending) and the conclusions indicate that imaging con be used to selectively identify patients that can avoid preop therapy. Roughly 60 % got preop therapy but it does not appear to be clearly defined what preop therapy was. Also there were a number of patients <T3. I have not seen much chatter about this study. I was wondering if anyone has heard this brought up at tumor board. It is very difficult to interpret the relevance.
There is a publication in the Annals of Surgery (not sure if more are pending) and the conclusions indicate that imaging con be used to selectively identify patients that can avoid preop therapy. Roughly 60 % got preop therapy but it does not appear to be clearly defined what preop therapy was. Also there were a number of patients <T3. I have not seen much chatter about this study. I was wondering if anyone has heard this brought up at tumor board. It is very difficult to interpret the relevance.
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
Mesorectal nodes are very hard to confirm preop.
Look at this 10-year-old study:
cT3N0 rectal cancer: potential overtreatment with preoperative chemoradiotherapy is warranted. - PubMed - NCBI
Despite neoadjuvant treatment 22% of initially cT3cN0 patients turned out to be ypN+.
Look at this 10-year-old study:
cT3N0 rectal cancer: potential overtreatment with preoperative chemoradiotherapy is warranted. - PubMed - NCBI
Despite neoadjuvant treatment 22% of initially cT3cN0 patients turned out to be ypN+.
A mesorectal/sacral recurrence is truly horrible, and typically neoadjuvant chemo xrt is not very toxic, if you make sure the anus is out of the field, and spare small bowel. I have no problem skimping on anterior coverage if worried about toxicity, and with the anus, I can usually spare some of it (get pet and mri to carefully define tumor) unless gross extension into anal canal.
(your major target is the mesorectum,posterior to the rectum- in fact the tumor is often the least important part of your ptv as it will come out with negative margins (unless it is T4 or near anal verge) the vast majority of recurrences are in mesorectum, followed by the anastomosis.
(your major target is the mesorectum,posterior to the rectum- in fact the tumor is often the least important part of your ptv as it will come out with negative margins (unless it is T4 or near anal verge) the vast majority of recurrences are in mesorectum, followed by the anastomosis.
Last edited:
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
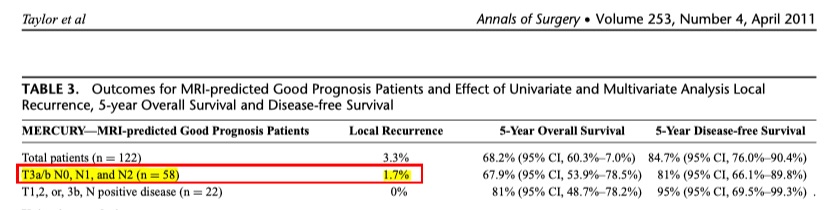
Mercury Study found "good prognosis" Stage III rectal ca had LR of 3%.
In T3a/b pts, LR was 1.7%.
No pts received pre or post op XRT.
All pts had TME.
THE MERCURY STUDY CAN BE FOUND HERE:
doi: 10.1097/SLA.0b013e31820b8d52
______________________________
_______________________________
In T3a/b pts, LR was 1.7%.
No pts received pre or post op XRT.
All pts had TME.
THE MERCURY STUDY CAN BE FOUND HERE:
Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study
doi: 10.1097/SLA.0b013e31820b8d52
______________________________
_______________________________
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Mercury Study found "good prognosis" Stage III rectal ca had LR of 3%.
In T3a/b pts, LR was 1.7%.
No pts received pre or post op XRT.
All pts had TME.
THE MERCURY STUDY CAN BE FOUND HERE:
Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study
doi: 10.1097/SLA.0b013e31820b8d52
View attachment 353135
______________________________
View attachment 353137
_______________________________
View attachment 353138
If LR without XRT in this group is 1.7-3.3%, what is the benefit of XRT?
PRODIGE 23 trial published in Lancet May 2021 states in the "Research in Context" section: "Preoperative short-course radiotherapy or long-course chemoradiotherapy reduces local recurrence rates from 25–40% to about 5%"
What does XRT do for someone whose risk is 1.7-3.3%?
- Joined
- Feb 7, 2019
- Messages
- 258
- Reaction score
- 804
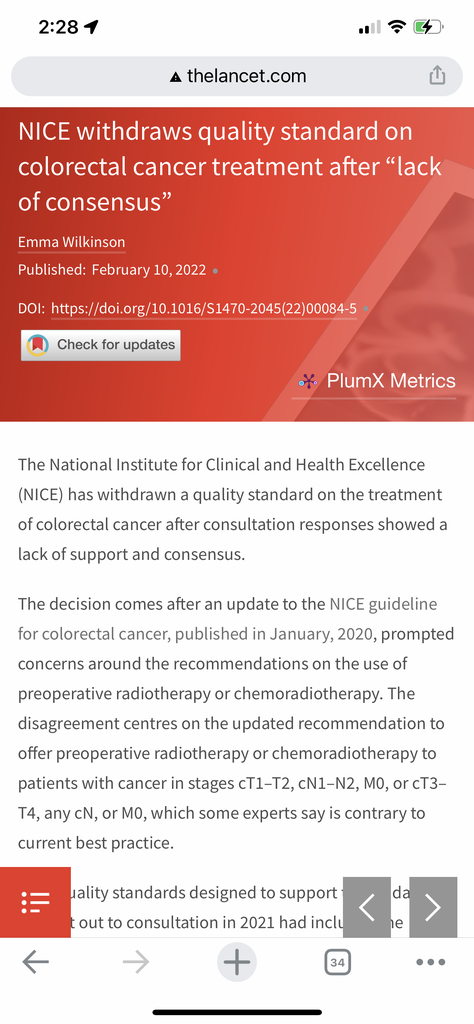
I believe the reason this paper from 2011 faded to obscurity is this randomized trial from UK showing that upfront surgery is less effective than neoadjuvant.If LR without XRT in this group is 1.7-3.3%, what is the benefit of XRT?
PRODIGE 23 trial published in Lancet May 2021 states in the "Research in Context" section: "Preoperative short-course radiotherapy or long-course chemoradiotherapy reduces local recurrence rates from 25–40% to about 5%"
What does XRT do for someone whose risk is 1.7-3.3%?

Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial
Taken with results from other randomised trials, our findings provide convincing and consistent evidence that short-course preoperative radiotherapy is an effective treatment for patients with operable rectal cancer.
www.thelancet.com
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
Which is of course total nonsense.PRODIGE 23 trial published in Lancet May 2021 states in the "Research in Context" section: "Preoperative short-course radiotherapy or long-course chemoradiotherapy reduces local recurrence rates from 25–40% to about 5%"
These are numbers predating modern TME and only for tumors with CRM involvement.
Last week's tumor board case:
EUS-staged cT3 cN0 tumor in the upper rectum, MRI showed minimal T3. No nodes, CRM will not be an issue.
Me and the med onc colleague wanted to do preop treatment, the surgeons wanted to resect.
I laid down all the evidence, stressed out that there's a 30%+ chance this will be an pN1 after surgery and the patient will need more intensive chemotherapy then, while if we downstage it now we will never have to suggest that postoperatively.
There's the wonderful MSKCC JCO-paper almost 15 years old, showing 20%+ chance of pN1 in cT3cN0 treated with neoadjuvant RCT.

cT3N0 rectal cancer: potential overtreatment with preoperative chemoradiotherapy is warranted - PubMed
The accuracy of preoperative ERUS/MRI for staging mid to distal cT3N0 rectal cancer is limited because 22% of patients have undetected mesorectal LN involvement despite CMT. Therefore, ERUS-/MRI-staged T3N0 rectal cancer patients should continue to receive preoperative CMT. Although 18% may be...
It still didn't work. They are going to resect the tumor without preoperative treatment.
I fear we are going to have another discussion if this comes back as pT3 pN1 (1/20) cM0 R0 (wide margins) concerning adjuvant treatment.
The data for postoperative RCT are worse and that patient will probably only get chemo (3 months of CAPOX or FOLFOX) then.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
I believe the reason this paper from 2011 faded to obscurity is this randomized trial from UK showing that upfront surgery is less effective than neoadjuvant.

Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial
Taken with results from other randomised trials, our findings provide convincing and consistent evidence that short-course preoperative radiotherapy is an effective treatment for patients with operable rectal cancer.www.thelancet.com
Looking at the MRC CR07 study:
Compared NeoAdj XRT for 624 pts vs PostOp XRT (approx. 69% with CTX) for 79 pts (spared 552 patients from XRT).
The 79 PostOp pts who received PostOp XRT was mostly due to a positive margin and were therefore all high risk.
In those 624 NeoAdj pts there was almost assuredly an unknown number of low risk patients who would not benefit from NeoAdj RT, i.e., some would have been found to be T1-2N0 had they been taken to surgery upfront. If true, the NeoAdj group was a lower risk group.
Therefore, didn't the two groups have differing risks of LR (the main outcome of the trial)?
If so, wouldn't one expect such a comparison to favor the NeoAdj group?
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Looking at the MRC CR07 study:
Compared NeoAdj XRT for 624 pts vs PostOp XRT (approx. 69% with CTX) for 79 pts (spared 552 patients from XRT).
The 79 PostOp pts who received PostOp XRT was mostly due to a positive margin and were therefore all high risk.
In those 624 NeoAdj pts there was almost assuredly an unknown number of low risk patients who would not benefit from NeoAdj RT, i.e., some would have been found to be T1-2N0 had they been taken to surgery upfront. If true, the NeoAdj group was a lower risk group.
Therefore, didn't the two groups have differing risks of LR (the main outcome of the trial)?
If so, wouldn't one expect such a comparison to favor the NeoAdj group?
Also, only 52% of pts on the MRC CR07 trial had TME so results very well may have differed due to surgical technique.
- Joined
- Apr 3, 2019
- Messages
- 4,278
- Reaction score
- 9,999
This is becoming a thing btw
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
xrt has a very tenuous role in GI.
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
Rectal, maybe? Still getting plenty of pancreas, goose and anal, not seeing how that goes awayxrt has a very tenuous role in GI.
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
Anal goes away with hpv. Pancreas, is the site with the least amount of evidence. As xrt retreats from the rest of gi, doubts abt pancreas will grow even larger.Rectal, maybe? Still getting plenty of pancreas, goose and anal, not seeing how that goes away
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
We'll still have all those oligomets in the abdomen, right?Anal goes away with hpv. Pancreas, is the site with the least amount of evidence. As xrt retreats from the rest of gi, doubts abt pancreas will grow even larger.
Right?
Cardiac ablation?
brb gonna go read KO Tweets
- Joined
- Apr 3, 2019
- Messages
- 4,278
- Reaction score
- 9,999
I bet I haven’t treated a “definitive” chemorads pancreas in 3 years. And thank goodness. I mean, we used to do a fair amount of those, right? I guess I have lost them to the academic centers doing high dose hypofx.Rectal, maybe? Still getting plenty of pancreas, goose and anal, not seeing how that goes away
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
if it is a high T3N0, some large volume centers like MSKCC may argue to omit radiation. I cant see anyone suggesting leaving it out for N1, although there is an intergroup study randomizing neoadjuvant xrt vs folfox presently.
ESMO Guidelines suggest it is appropriate to consider omitting PostOp XRT/CTX in N1, as long as pt has appropriate TME:
"Postoperative chemoradiotherapy. Preoperative CRT (i.e. 4554 Gy, 1.8–2.0 Gy/fraction) or SCPRT has better outcomes than postoperative CRT [87, 88]. Traditionally, postoperative CRT was administered for all patients with pT3-4 or pN þ tumours, and combined with additional 4 months of adjuvant bolus 5-FU ChT, but the routine use of CRT to reduce local recurrence can be questioned if a good-quality TME can be assured [53]."
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
Using ESMO guidelines in the US..... should go over well in front of a jury.ESMO Guidelines suggest it is appropriate to consider omitting PostOp XRT/CTX in N1, as long as pt has appropriate TME:
"Postoperative chemoradiotherapy. Preoperative CRT (i.e. 4554 Gy, 1.8–2.0 Gy/fraction) or SCPRT has better outcomes than postoperative CRT [87, 88]. Traditionally, postoperative CRT was administered for all patients with pT3-4 or pN þ tumours, and combined with additional 4 months of adjuvant bolus 5-FU ChT, but the routine use of CRT to reduce local recurrence can be questioned if a good-quality TME can be assured [53]."
View attachment 353173
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Probably a Catch 22.Using ESMO guidelines in the US..... should go over well in front of a jury.
D
deleted1111261
Agree. pN1 - NCCN does not mention observation as an option.Using ESMO guidelines in the US..... should go over well in front of a jury.
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
I agree. Larger issue is where this field is headed. Scarcely a week goes by without something like this coming out.Using ESMO guidelines in the US..... should go over well in front of a jury.
- Joined
- Mar 14, 2002
- Messages
- 14,926
- Reaction score
- 8,917
I bet I haven’t treated a “definitive” chemorads pancreas in 3 years. And thank goodness. I mean, we used to do a fair amount of those, right? I guess I have lost them to the academic centers doing high dose hypofx.
Had a pancreatic surgeon in the lunch line at my academic center recently yelling at me that there's no role for radiation in pancreas.
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
Had a pancreatic surgeon in the lunch line at my academic center recently yelling at me that there's no role for radiation in pancreas.
Not totally right but not totally wrong either
- Joined
- Sep 20, 2004
- Messages
- 11,778
- Reaction score
- 11,867
So localized unresectable gets gem abraxane or folfirinox and then goes to hospice?Had a pancreatic surgeon in the lunch line at my academic center recently yelling at me that there's no role for radiation in pancreas.
- Joined
- Apr 3, 2019
- Messages
- 4,278
- Reaction score
- 9,999
Really the only comeback we can make:Had a pancreatic surgeon in the lunch line at my academic center recently yelling at me that there's no role for radiation in pancreas.

Lunch lines gettin brutal in academic rad onc. See you at the breadline @thecarbonionangle
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
Certainly that’s what most the trials support. I give the old college try in tumor board, but can’t make a strong argument against this.So localized unresectable gets gem abraxane or folfirinox and then goes to hospice?
- Joined
- Mar 14, 2002
- Messages
- 14,926
- Reaction score
- 8,917
So localized unresectable gets gem abraxane or folfirinox and then goes to hospice?
First one then the other.
I'm sure they're still doing IRE with the biopsy beforehand though. Radiation bad. Surgery good. Right?
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
So localized unresectable gets gem abraxane or folfirinox and then goes to hospice?
no i think reasonable to offer radiation if not progressing after above chemo regimens. are we just treating ourselves? maybe. but yeah I think that makes sense to me.
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
Of course it is reasonable. Just not what the best evidence shows, so if a medonc objects, we don’t have much of a leg to stand on.no i think reasonable to offer radiation if not progressing after above chemo regimens. are we just treating ourselves? maybe. but yeah I think that makes sense to me.
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
Of course it is reasonable. Just not what the best evidence shows, so if a medonc objects, we don’t have much of a leg to stand on.
Well we don’t have evidence in that exact scenario, which is why people do it.
We know from LAP07 that chemo vs chemoRT there is no OS difference. What I’m talking about is a little bit different.
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
Agreed, not exactly same scenario, but anyone failing first line treatment has horrible prognosis and local treatment almost certainly won’t make measurable difference. Look, I do it - just playing devils advocate.
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,263
Agreed, not exactly same scenario, but anyone failing first line treatment has horrible prognosis and local treatment almost certainly won’t make measurable difference. Look, I do it - just playing devils advocate.
You’re making my exact point! Agree - if someone is progressing on chemo, then that’s different.
But stable locally and distantly on chemo for some time? Then reasonable to try local RT. Upfront chemoRT for all isn’t really a great idea, per LAP07. So how
About using chemo to pick out the winners.
- Joined
- Oct 4, 2017
- Messages
- 5,037
- Reaction score
- 9,836
Again agree with you. But can’t change medonc opinions. Just don’t see many pts.
- Joined
- Dec 2, 2011
- Messages
- 1,494
- Reaction score
- 3,034
I don’t see this being a real issue in the US. The US and Europeans are really diverging on rectal cancer with the former moving towards TNT +/- surgery whereas the latter solidly views this as a surgical disease.I agree. Larger issue is where this field is headed. Scarcely a week goes by without something like this coming out.
I’ll admit, I bet good surgery and chemo alone is probably sufficient for N1 disease but I would need better data, not hypothetical reasoning, to convince me to change practice. Especially since it contradicts US guidelines.
- Joined
- Oct 19, 2004
- Messages
- 536
- Reaction score
- 833
Kennedy et al looked at what patients thoughts were re: PreOp CTX/RT in rectal ca:
54% of future patients would not choose CRT until it offered an absolute reduction in LR from 15% to 5% or less.
DOI: 10.1002/cncr.25842
Cancer, July 1, 2011
"Give the People What They Want"

54% of future patients would not choose CRT until it offered an absolute reduction in LR from 15% to 5% or less.
DOI: 10.1002/cncr.25842
Cancer, July 1, 2011
"Give the People What They Want"
D
deleted1111261
Hmm. Wonder if anyone would accept that recurrence rate having experienced a sacral recurrence? That can be incredibly painful...
- Joined
- Apr 3, 2019
- Messages
- 4,278
- Reaction score
- 9,999
"I will choose to irradiate nodes in all N+ women to get the LRR from 7.8% to 4.8% at 10 years" - all Rad Oncs54% of future patients would not choose CRT until it offered an absolute reduction in LR from 15% to 5% or less.
Sorry it's Monday and I haven't had my tuna fish and cigarettes yet
Similar threads
- Replies
- 56
- Views
- 3K
