Well, if that's the explanation, then why don't the majority of the other phase III trials on hypofractionation show a diference in late toxicity?
What's so different about this trial?
Help me understand why 68 Gy in 25 fractions to the rectum are worse than 78 Gy in 39 fractions, when at the same time 60 Gy in 20 fractions were not worse than 74 Gy in 37 fractions (CHHiP). You are saying that it has to do with treating the nodes, but how does this work from the radiation biology point of view?
Because there is a lot we don't know about rectal constraints and toxicity.
What if the V40 of rectum over 25 fractions, when combined with a V60 in 25 fractions, are both necessary to be elevated to put patient at risk for late toxicity? This is something that would be seen only in this trial and NOT in CHhiPP
I don't know the answer as to WHY. The above is wild speculation. I know the answer is that based on our current evidence base, it DID.
And to have an entire specialty continue to state that things that exist, in randomized data, try to definitively state that it simply CANNOT be true because it does not agree with our pre-conceived notions and things that we think we know based on previous similar (but NOT identical) trial data, is the worst type of dogma we can practice.
Before this trial, I thought "mod hypo to the prostate has only been studied in prostate only patients, but meh, 45-50Gy in 25-28fx, probably fine, we do it when doing sequential boosts, in other pelvic cancers (even with chemo!), it's probably fine"
Now we have randomized data, which is one data point, predicting a 14%(!) G3+ late GI toxicity rate, reportedly driven by rectal bleeding.
Maybe the Canadians are super quick to Argon Plasma Coagulation or other procedural intervention (which would be CTCAE G3 tox) on anyone with rectal bleeding.
All I know is that the Canadians are incentivized to prove that everything is safer to be given faster (just like the UK), to the point where they treated the mod hypo patients with fiducials, better immobilization, smaller margins, and more frequent IGRT.
And Mod hypo STILL LOST the toxicity battle.
But because this goes against the dogma that has been pushed so fervently over the past 2-3 decades in prostate cancer.... suddenly it's the trial's fault? We're going to ignore and keep doing things the way we used to?
Ask yourself why you (both Palex as well as the 'proverbial' you to those reading) are so resistant to even considering changing practice based on this trial.
Just imagine with me for a second - if results were reversed, where conventional Fx caused MORE late toxicity, would that not be a nail in the coffin of conventional Fx (the way 40/15 for WBI has LESS toxicity than 50/25 Fx WBI)?
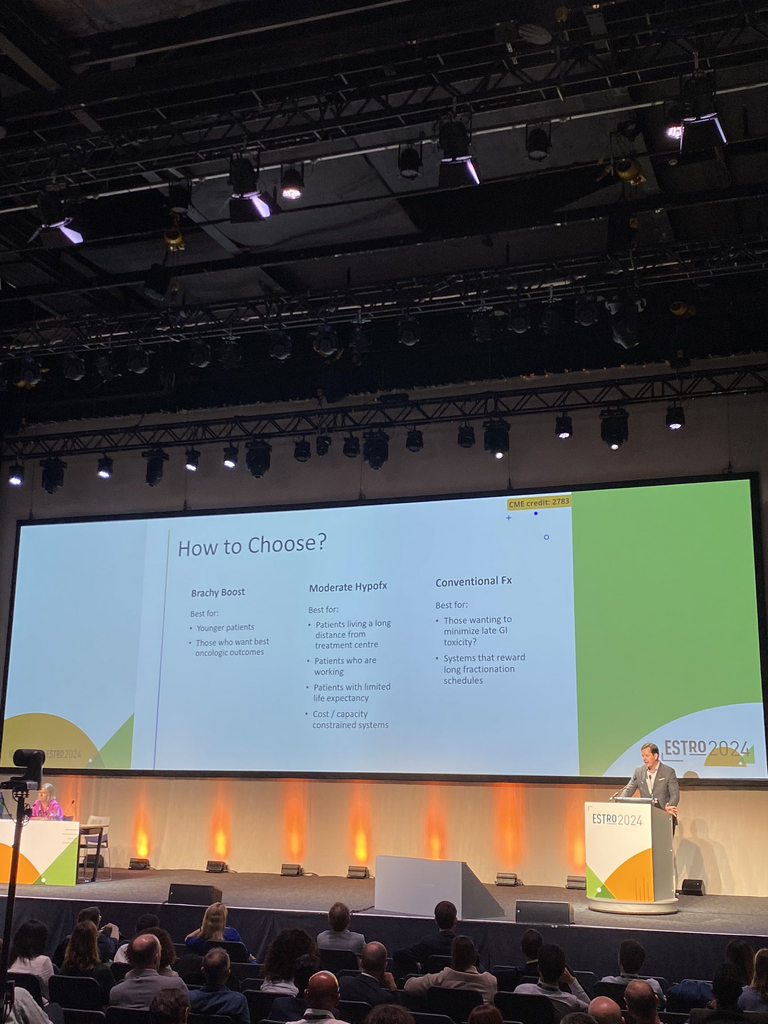
I'm not saying no patient should ever be treated with a mod hypo regimens with nodes again. If a patient who needs nodes radiated wants a faster treatment and is willing to accept toxicity difference, then sure. But we had equipoise in the setting of NO ENI data. And now we have data that offends our sensibilities. And we're going to choose to ignore it?
C'mon man.