- Joined
- Jul 2, 2013
- Messages
- 11,517
- Reaction score
- 15,414
Kind of weird to me that we're discussing this as if augmentation is the preferred method as I generally like to avoid polypharmacy as much as possible. If we're talking depression I will often switch to another agent like SNRI, TCA, or others before augmenting if there's not an adequate response or patients have notable side effects.What are your top 7 ssri augmentation agents
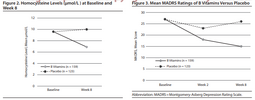
For actual depression augmentation: therapy, wellbutrin, mirtazapine, trazodone (I also like nefazodone, but don't use it much), lithium/abilify/other SGA (preferably a partial agonist). If mild to moderate depression I also strongly emphasize regular physical activity. After that it's a crap shoot and we can throw in lamotrigine, high doses of buspar, thyroid hormone, low dose stimulants/modafinil, phototherapy, or even some supplements/vitamins (vit d, n-acetylcysteine, omega-3's, etc). I wish amisulpride was available in the US, as that would be a potential option in a lot of cases (depression or otherwise).
Like most other psych conditions, I may choose to utilize some options before others if there's other indications for one over another and trying to boil down psychiatry to some kind of cook-book algorithm based on a DSM diagnosis is only helpful for relatively basic cases where formulation isn't really all that necessary. By the time we're getting to "treatment resistant depression" (I mean real TRD, not the insurance definition of 'has failed 3 meds') it gets too complex to stick to a script of medications for longer-term treatment. I also prefer options that have stronger evidence of decent effect sizes than options with weaker evidence for most patients.