This was briefly touched on before some classic SDN s*** flinging started, but how do you all feel about the numerous IM/FM trained doctors that are more or less acting as an “intensivist-lite” at critical access hospitals? I have seen literally hundreds of locums and FT job postings that have in the requirements: open ICU, must be comfortable managing ICU patients, intubation, central/art lines, vent management required.
Not saying doing those procedures = being a true CCM doctor, but it seems like FM/IM are already practicing aspects of critical care medicine in the community. Should it be this way? Probs not but it is a reality and cheap hospital admin isn’t going to stop requiring it anytime soon, so why not let FM doctors with equivalent ICU and inpatient time an EM/IM do a CC fellowship?
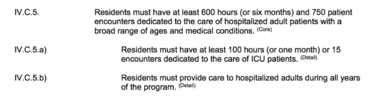
There are multiple threads about IM residents getting <10 intubations, central/art, etc by PGY3. Counter argument is that they probably wouldn’t be competitive for critical care fellowship since they most likely didn’t do extra ICU time. But, it does open up the argument that a motivated FM resident at an unopposed program could easily surpass an IM resident in both critical care procedures and ICU time. No way any FM resident is going to match IM in terms of inpatient months (30+ months I think?), but that is true for EM too, which already struggles to get 6 months of ICU experience before CC fellowship.
I will defer to actual critical care doctors on what they think is most important coming into a CC fellowship…procedural experience? ICU experience? Non-ICU inpatient experience?
I’m not remotely qualified to say what is most important and how much time/experience in each is needed, but I can say that an unopposed FM resident could get similar procedures and ICU time to an IM/EM resident.