For those of you who see a lot of high risk prostate cancer. Say you are treating prostate 60Gy/20 and bilateral nodal regions to 44Gy/20 via SIB. Which of the subvolmes includes SV? Thanks
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Dose-painting seminal vesicles
- Thread starter seper
- Start date
- Joined
- Apr 21, 2011
- Messages
- 3,627
- Reaction score
- 9,284
I do first 1-2 cm to 60 and the rest to the intermediate dose.
Edit: unless evidence of involvement on imaging
Edit: unless evidence of involvement on imaging
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
I usually do 70/28 (just personal preference, easier to follow constraints, etc.), and when I do, I do 70Gy to Prostate + Prox 1cm, then 56 to remainder of SV (in HR patients), then 50.4 to pelvic nodes.
- Joined
- May 7, 2014
- Messages
- 1,659
- Reaction score
- 3,479
If 60/20 to prostate (and MRI+SV)
50 Gy to entire SV
50 Gy to entire SV
- Joined
- Oct 4, 2017
- Messages
- 5,035
- Reaction score
- 9,831
I just include 1 cm of seminal vesicles and don’t dose paint. Almost all sv invasion is within .3 cm of prostate.
- Joined
- Apr 3, 2019
- Messages
- 4,276
- Reaction score
- 9,995
Only case like this I ever had. Once saw a guy who had RP by the chair of urology Miami few years prior. Had a rising PSA. Did an MRI. Very suspicious finding in SVs. I was surprised… don’t you always remove SVs w/ an RP?? Evidently not. Read the op report… no mention of SVs coming out. (No super high risk features on path.) I consulted my local urologist and had him do directed biopsy of the SVs … in the juicy part. Lo and behold was positive. IMRTd it with high dose and short course AAT.I just include 1 cm of seminal vesicles and don’t dose paint. Almost all sv invasion is within .3 cm of prostate.
- Joined
- Apr 21, 2011
- Messages
- 3,627
- Reaction score
- 9,284
I see a lot of remnant SVs and always cover them when giving post-op
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Since I know this question is a hill which many Radiation Oncologists will eagerly climb to spill their blood while defending their opinion, let me preface this by saying: I don't think there is a "right" answer, I just genuinely want to hear thoughts. This question of SV painting is a good jumping off point, because I've had this conversation recently and I find it interesting.
My Google search history is littered with the phrase: "high risk prostate cancer hypofrac data". I probably search at least once a week, looking for...I don't know. The Answer, I guess.
For those of you who are treating high risk or very-high risk prostate cancer, including nodes, with 70/28 or 60/20: why?
I don't feel like Googling again but weren't only ~120 CHHiP patients high risk? I think the data is bountiful for low and intermediate risk, obviously. But if you put a gun to my head and demanded I justify hypofrac for high risk with covering nodes, I don't know if I can weave together a compelling argument knowing that many of these trials either didn't have high risk patients or only had a few of them.
But, I've watched some of you author compelling treatment justifications in a single paragraph so...can someone help me give Google and PubMed a break for at least a month? The internet is tired of me asking.
My Google search history is littered with the phrase: "high risk prostate cancer hypofrac data". I probably search at least once a week, looking for...I don't know. The Answer, I guess.
For those of you who are treating high risk or very-high risk prostate cancer, including nodes, with 70/28 or 60/20: why?
I don't feel like Googling again but weren't only ~120 CHHiP patients high risk? I think the data is bountiful for low and intermediate risk, obviously. But if you put a gun to my head and demanded I justify hypofrac for high risk with covering nodes, I don't know if I can weave together a compelling argument knowing that many of these trials either didn't have high risk patients or only had a few of them.
But, I've watched some of you author compelling treatment justifications in a single paragraph so...can someone help me give Google and PubMed a break for at least a month? The internet is tired of me asking.
- Joined
- Feb 9, 2020
- Messages
- 107
- Reaction score
- 172
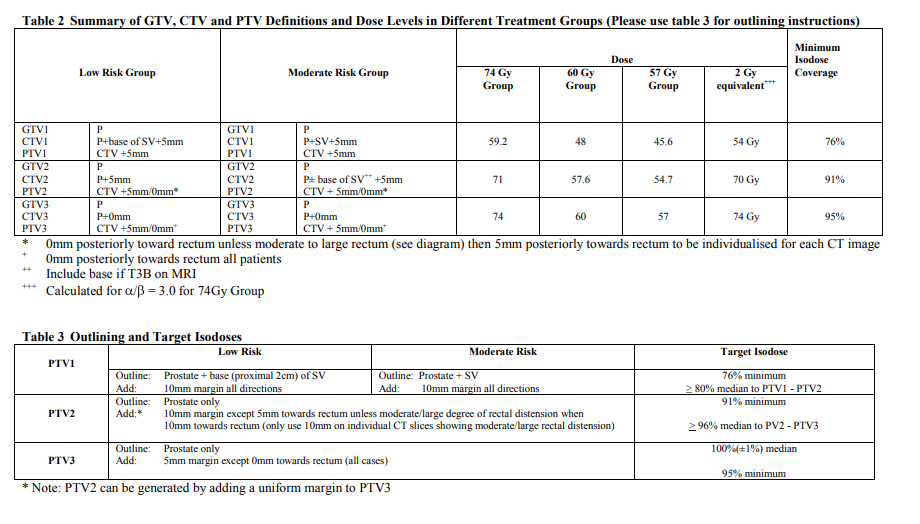
You could dose paint proximal 2 cm SV to 57.6, (48 to remaining SV) like the original protocol, or just to 60 since it's probably an inconsequential difference.
- Joined
- Aug 6, 2013
- Messages
- 416
- Reaction score
- 681
I haven't seen anything that suggests hypofx has inferior outcomes. There is this small exclusively high risk trial (using 3DCRT) that showed superior outcomes with hypofx. Good PS patients get brachy in our group but the others mostly get hypofx. Nothing wrong with standard fx either but for me it's kinda like when breast was starting to get hypofractionated and we would hold out on triple neg, large separation, prior chemo etc but now they all by and large get hypofx. I'd just be shocked if there were worse oncologic outcomes in any sort of (non FLAME style) conv vs hypo study.Since I know this question is a hill which many Radiation Oncologists will eagerly climb to spill their blood while defending their opinion, let me preface this by saying: I don't think there is a "right" answer, I just genuinely want to hear thoughts. This question of SV painting is a good jumping off point, because I've had this conversation recently and I find it interesting.
My Google search history is littered with the phrase: "high risk prostate cancer hypofrac data". I probably search at least once a week, looking for...I don't know. The Answer, I guess.
For those of you who are treating high risk or very-high risk prostate cancer, including nodes, with 70/28 or 60/20: why?
I don't feel like Googling again but weren't only ~120 CHHiP patients high risk? I think the data is bountiful for low and intermediate risk, obviously. But if you put a gun to my head and demanded I justify hypofrac for high risk with covering nodes, I don't know if I can weave together a compelling argument knowing that many of these trials either didn't have high risk patients or only had a few of them.
But, I've watched some of you author compelling treatment justifications in a single paragraph so...can someone help me give Google and PubMed a break for at least a month? The internet is tired of me asking.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
I'm not super familiar with that paper, I need to dig into it. My immediate reaction from the abstract is 1) it's 3D, 2) it's from 2003-2007 which might have other implications about technology/support/workflows etc, 3) it used 9 months of ADT, 4) it has only 3 years of follow-up. I'm curious if they have longer follow-up publications now.I haven't seen anything that suggests hypofx has inferior outcomes. There is this small exclusively high risk trial (using 3DCRT) that showed superior outcomes with hypofx. Good PS patients get brachy in our group but the others mostly get hypofx. Nothing wrong with standard fx either but for me it's kinda like when breast was starting to get hypofractionated and we would hold out on triple neg, large separation, prior chemo etc but now they all by and large get hypofx. I'd just be shocked if there were worse oncologic outcomes in any sort of (non FLAME style) conv vs hypo study.
So, yes, it does strike me as the breast and chemo example. However, in my view, one of the core justifications for hypofrac in prostate is the low alpha/beta produced by the long doubling time of prostate cancer cells. Is it an unreasonable leap to assume that high Gleason grade cancers might have a shorter doubling time, and therefore a higher alpha/beta, and a suboptimal response to big fraction sizes?
Obviously a lot of other factors go into this, but that's sort of where my brain goes.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Also, I'm aware that I should follow my comment up with checking out the basic science literature for alpha/beta values in high Gleason grades, if such a paper exists, but it's been a long day and I just can't muster the energy.
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
This is one of this "urban myths" of radiation oncology. It's quite possible that high gleason score is associated with a higher a/b, however in subgroup analyses of the randomized trials testing hypofractionation vs. normofractionation, no signs of worse outcomes with hypofractionation in high gleason scores were shown.Also, I'm aware that I should follow my comment up with checking out the basic science literature for alpha/beta values in high Gleason grades, if such a paper exists, but it's been a long day and I just can't muster the energy.
The same also applies for breast cancer. We never saw that G3 tumors, for instance, fare worse with hypofractionation than with normofractionation and the hypofractionation trials on breast cancer also assumed a low a/b for breast cancer cells.
What potentially can be explanation for this,:
1. Any effect on less favorable local control with hypofractionation in aggresive forms of prostate and breast cancer does not pop up in PFS/OS-graphs, because these patients are also at high risk of systemic progression, irrelevant of local control. Thus, whether or not you eradicate all cancer cells in the prostate or lumpectomy cavity is irrelevant, since these patients are already micrometastatic.
2. Systemic treatment, which is generally intensified in these patients (long term ADT / chemotherapy), manages to close the gap in less favorable local control.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Are you TRYING to summon the ghosts of Radiation Biologists with that statement? It's Christmas, not Halloween. Check your calendar!This is one of this "urban myths" of radiation oncology. It's quite possible that high gleason score is associated with a higher a/b, however in subgroup analyses of the randomized trials testing hypofractionation vs. normofractionation, no signs of worse outcomes with hypofractionation in high gleason scores were shown.
The same also applies for breast cancer. We never saw that G3 tumors, for instance, fare worse with hypofractionation than with normofractionation and the hypofractionation trials on breast cancer also assumed a low a/b for breast cancer cells.
What potentially can be explanation for this,:
1. Any effect on less favorable local control with hypofractionation in aggresive forms of prostate and breast cancer does not pop up in PFS/OS-graphs, because these patients are also at high risk of systemic progression, irrelevant of local control. Thus, whether or not you eradicate all cancer cells in the prostate or lumpectomy cavity is irrelevant, since these patients are already micrometastatic.
2. Systemic treatment, which is generally intensified in these patients (long term ADT / chemotherapy), manages to close the gap in less favorable local control.
On a serious note...those are excellent points. In digesting that with my internal narrative re: how I think about prostate, your two statements fit in nicely with my own cancer heuristics.
I treat a lot of prostate, and as I'm sure we all know, prostate patients can be a special breed. Over the last few weeks, two of my patients in particular had that "secret sauce" of being smart, having knowledge/experience in Oncology-adjacent fields, and demonstrating extremely high anxiety about their diagnosis, which they deal with by engaging rationalization/intellectualization defense mechanisms.
Thus, at every interaction from consult to the end of treatment, they come at me with these well-crafted questions that I try to answer in layman's terms. I have basically given these two an "explain like I'm five" verbal history of prostate cancer from the 1980s to now. Fortunately, neither are high risk so this doesn't apply to them. However, it occurred to me that if they WERE high risk, I don't know if I could give them a convincing argument about "hypofrac for high risk prostate", given 1) the incongruence in the radiation biology justifications and 2) the lack of inclusion of these patients in the non-inferiority trials.
Anyway, my ears (eyes? I guess I read posts) remain open to other justifications for hypofrac in high risk, to save myself from future OTV battles and help me sleep at night.
- Joined
- Jul 26, 2007
- Messages
- 12,695
- Reaction score
- 2,317
Seems like you answered the question yourself - in lieu of incredibly convincing data, hypofractionate the annoying patients and standard frac the cool ones
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
I choose a middle way out of this dillema.However, it occurred to me that if they WERE high risk, I don't know if I could give them a convincing argument about "hypofrac for high risk prostate", given 1) the incongruence in the radiation biology justifications and 2) the lack of inclusion of these patients in the non-inferiority trials.
I treat patients with high-risk disease without major comorbidities with electiv pelvic RT with conventional fractionation, the boost the prostate with hypofractionation.
For instance pelvis + prostate 50.4/1.8 followed by prostate 24/3. That comforts me.
- Joined
- Apr 3, 2019
- Messages
- 4,276
- Reaction score
- 9,995
The same also applies for breast cancer. We never saw that G3 tumors, for instance, fare worse with hypofractionation than with normofractionation
This is one of this "urban myths" of radiation oncology. It's quite possible that high gleason score is associated with a higher a/b
The data is not 100% pure in supporting your two propositions for breast and prostate respectively. It's mostly pure but not totally pure. I could put forward some arguments... which could easily be counter-argued. IMHO, I think it's very possible higher Gleason has higher a/b. Look at the a/b 95% C.I.'s in papers that try to solve the a/b prostate problem. TBH I think looking at things like G3 and Ki67 in regards to a/b in breast cancer is under-studied. Gleason's and grading are crude tools but likely rough surrogates for "biomolecularaties" which almost certainly heterogenize a/b in individual disease sites.I treat patients with high-risk disease without major comorbidities with electiv pelvic RT with conventional fractionation,
AND then at the end you conventionally fractionate the nodes. Ha. We know the lion by his claw.
- Joined
- Oct 4, 2017
- Messages
- 5,035
- Reaction score
- 9,831
I hypofract pts who live far away. Conventional for rest.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
This is how I am currently choosing to practice as well (for high and very high risk).I hypofract pts who live far away. Conventional for rest.
I am very familiar with the hypofrac boost regimen @Palex80 uses, and know a lot of folks who do the same. Ultimately (for now), I decided against using it because it feels like it's cobbling together multiple theories to create an untested permutation, and it felt more "stable" either go with "regular" hypofrac or conventional schemes (as in, when conducting an experiment and evaluating an outcome, it's best to alter only one variable at a time).
And yes, I may end up choosing schemes by a complicated algorithm involving the AUC of personality * frequency of OTVs.
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
The data is not 100% pure in supporting your two propositions for breast and prostate respectively. It's mostly pure but not totally pure. I could put forward some arguments... which could easily be counter-argued. IMHO, I think it's very possible higher Gleason has higher a/b. Look at the a/b 95% C.I.'s in papers that try to solve the a/b prostate problem. TBH I think looking at things like G3 and Ki67 in regards to a/b in breast cancer is under-studied. Gleason's and grading are crude tools but likely rough surrogates for "biomolecularaties" which almost certainly heterogenize a/b in individual disease sites.
AND then at the end you conventionally fractionate the nodes. Ha. We know the lion by his claw.
- Joined
- May 7, 2014
- Messages
- 1,659
- Reaction score
- 3,479
Why not go all the way? Instead of 4-5 weeks howsabout 4-5 treatments?Since I know this question is a hill which many Radiation Oncologists will eagerly climb to spill their blood while defending their opinion, let me preface this by saying: I don't think there is a "right" answer, I just genuinely want to hear thoughts. This question of SV painting is a good jumping off point, because I've had this conversation recently and I find it interesting.
My Google search history is littered with the phrase: "high risk prostate cancer hypofrac data". I probably search at least once a week, looking for...I don't know. The Answer, I guess.
For those of you who are treating high risk or very-high risk prostate cancer, including nodes, with 70/28 or 60/20: why?
I don't feel like Googling again but weren't only ~120 CHHiP patients high risk? I think the data is bountiful for low and intermediate risk, obviously. But if you put a gun to my head and demanded I justify hypofrac for high risk with covering nodes, I don't know if I can weave together a compelling argument knowing that many of these trials either didn't have high risk patients or only had a few of them.
But, I've watched some of you author compelling treatment justifications in a single paragraph so...can someone help me give Google and PubMed a break for at least a month? The internet is tired of me ask
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Uggh I know, I know.
I can see reaching a point in the near future where I need to block 2 hours for a prostate consult if I have a hope of having a true "shared decision making" conversation about ADT, SpaceOAR, and treatment scheme.
- Joined
- Oct 4, 2017
- Messages
- 5,035
- Reaction score
- 9,831
I am sure almost all prostate pts can be treated w/just 4-5 fractions, but then we would loose staff and resources.
Fortunately, nearby pps exempt center not big on hypof (despite seminal publications), so not under much competitive pressure yet.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
You know...for all the saber rattling in the literature and on Twitter, sure seems like a lot of folks are still using conventional (I see it a lot on my geographic area, too).Fortunately, nearby pps exempt center not big on hypof (despite seminal publications), so not under much competitive pressure yet.
To be clear, I am totally fine with conventional. It has the "best" evidence (by definition, as all hypofrac has is statisticians proclaiming it to be non-inferior by pre-specified analytics). What I am not fine with is publicly engaging in fraction shaming and then quietly doing conventional anyway.
I'm not big on the "do as I say, not as I do" attitude, in general.
D
deleted171718
For those of you who are treating high risk or very-high risk prostate cancer, including nodes, with 70/28 or 60/20: why?
Some of the best evidence for treating nodes in high-risk prostate cancer comes from POP-RT.
Last edited by a moderator:
D
deleted1111261
Can we bill that 3 fractions as an SBRT boost stateside ?I choose a middle way out of this dillema.
I treat patients with high-risk disease without major comorbidities with electiv pelvic RT with conventional fractionation, the boost the prostate with hypofractionation.
For instance pelvis + prostate 50.4/1.8 followed by prostate 24/3. That comforts me.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Excellent point!Some of the best evidence for treating nodes in high-risk prostate cancer comes from POP-RT. Patients in POP-RT were treated with hypofractionation (conventional dose to nodes). While not a fractionation comparison, if treating nodes, one could argue this is the best evidence for doing so
(Nothing against conventional fractionation... except maybe the alpha/beta argument).
- Joined
- Apr 3, 2019
- Messages
- 4,276
- Reaction score
- 9,995
Thou shalt not SBRT boost.Can we bill that 3 fractions as an SBRT boost stateside ?
- Medicare, Evicore, etc
- Joined
- Oct 10, 2011
- Messages
- 8,639
- Reaction score
- 10,742
I see 70/28x as conventional fractionation. Just like Canadian breast regimen
No. Increased risk of acute GI toxicity separates it from THE standard for me.
I think he means 24Gy in 8Fx of 3Gy a piece. Took me a while to learn how Palex writes his scripts.Can we bill that 3 fractions as an SBRT boost stateside ?
No harm in doing hypofx when doing nodes, but minimal comparison data.
D
deleted1111261
Oh! I thought 24 / 3No. Increased risk of acute GI toxicity separates it from THE standard for me.
I think he means 24Gy in 8Fx of 3Gy a piece. Took me a while to learn how Palex writes his scripts.
No harm in doing hypofx when doing nodes, but minimal comparison data.
sneaky palex
8/1 has less acute toxicity than 30/10, but which one is standard again??
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
You are all confusing me!Oh! I thought 24 / 3
sneaky palex
8/1 has less acute toxicity than 30/10, but which one is standard again??
I will start writing it the other way around...
So, it's 28 x 1.8 Gy followed by 8 x 3 Gy for the prostate.
- Joined
- Sep 20, 2004
- Messages
- 11,775
- Reaction score
- 11,866
Yet it couldn't make the cut for "choosing wisely" .... Guess that retreatment rate difference mattered to someoneOh! I thought 24 / 3
sneaky palex
8/1 has less acute toxicity than 30/10, but which one is standard again??
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Well, dovetailing nicely with this thread, the full publication is out, throwing in another wrinkle:
I have to go down the complicated VPN tunnel to get the full paper and haven't done so yet, but I assume all of these patients got 55/20? Or did this subset of patients get a different regimen?
I have to go down the complicated VPN tunnel to get the full paper and haven't done so yet, but I assume all of these patients got 55/20? Or did this subset of patients get a different regimen?
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
No, the publications refers to the M0 cohort of STAMPEDE. There are two main cohorts in STAMPEDE:I have to go down the complicated VPN tunnel to get the full paper and haven't done so yet, but I assume all of these patients got 55/20? Or did this subset of patients get a different regimen?
- locally advanced N1/N0 (if N0, two out of three criteria must be met: T3/4, GS 8-10, PSA >39)
- metastastic M1
These patients are the first cohort and received standard, normofractionated radiotherapy of the prostate +/- pelvis
2018-version of the protocol is available here.
55/20 or 36/6 were for the M1 cohort (STAMPEDE Arm H).
Last edited:
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Don't reward my laziness! But I appreciate you digging this out.No, the publications refers to the M0 cohort of STAMPEDE. There are two main cohorts in STAMPEDE:
- locally advanced N0/N1
- metastastic M1
These patients are the first cohort and received standard, normofractionated radiotherapy of the prostate +/- pelvis
2018-version of the protocol is available here.
View attachment 347169
View attachment 347170
It's not clear from the abstract of the full publication, but hopefully there was a predominant radiation scheme used? I suspect it will be a nice mix of conventional and hypofrac, nodal coverage or not, and continue the confusion.
Do you do 7 Gy x 10 for LN+ H&N cancer? If a/b is just a scam, all that should matter is total dose 😜
- Joined
- Dec 17, 2007
- Messages
- 3,413
- Reaction score
- 4,444
10 x 7 Gy for HNSCC sounds like an excellent regime. It will lead to very high local control rates.Do you do 7 Gy x 10 for LN+ H&N cancer? If a/b is just a scam, all that should matter is total dose 😜
With a high enough dose of RT, you can kill just about anything10 x 7 Gy for HNSCC sounds like an excellent regime. It will lead to very high local control rates.
- Joined
- Dec 2, 2011
- Messages
- 1,492
- Reaction score
- 3,031
Except for tardigrades apparently.With a high enough dose of RT, you can kill just about anything
But yes, this is part of my routine consult discussion for diseases like pancreatic cancer to explain why I can’t give enough radiation to get rid of the cancer. “I can give you enough to guarantee you don’t die of cancer, but that kinda defeats the purpose.”
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
Except for tardigrades apparently.
- Joined
- Dec 2, 2011
- Messages
- 1,492
- Reaction score
- 3,031
They actually can quite literally walk through that valley…

This Is How Tardigrades Walk, And We Were Not Ready For The Footage
Tardigrades are undoubtedly weird.
- Joined
- Nov 2, 2019
- Messages
- 3,507
- Reaction score
- 14,562
You sure do know a lot about tardigrades...They actually can quite literally walk through that valley…

This Is How Tardigrades Walk, And We Were Not Ready For The Footage
Tardigrades are undoubtedly weird.www.sciencealert.com
D
deleted1111261
time to break out Tardigrade into separate thread ?
- Joined
- Sep 20, 2004
- Messages
- 11,775
- Reaction score
- 11,866
Can't be the only trek nerd on here making the connection to star trek discovery...

 www.dailystartreknews.com
www.dailystartreknews.com

Dismissal of “Tardigrades” copyright lawsuit against CBS and Star Trek: Discovery has been upheld in appeal — Daily Star Trek News
The appeal filed by game developer Anas Abdin in a copyright infringement lawsuit against CBS has been dismissed by a judge in the United States Court of Appeals, Second Circuit, upholding an earlier decision to dismiss the case. Abdin sued both CBS and Netflix in 2018, alleging that the use of
- Joined
- Dec 2, 2011
- Messages
- 1,492
- Reaction score
- 3,031
“How do you know so much about tardigrades?”You sure do know a lot about tardigrades...
“You have to know these things when you are king. “
King Arthur to Sir Bedevere
- Joined
- Oct 4, 2017
- Messages
- 5,035
- Reaction score
- 9,831
Tardi

 www.discovermagazine.com
www.discovermagazine.com
You sure do know a lot about tardigrades...

How a Tardigrade "Micro Animal" Became Quantum Entangled with Superconducting Qubit
Physicists have extended the conditions in which life can exist further than ever before.
