CArdiac is probably the only subsecialty of anesthesia where CRNAs aren’t a threat and never will be. As old heart surgeons retire and new school surgeons arrive, the demand for consultant level subspecialty MD expertise will increase, compounded further by the growth of TEE guided structural.
Where I work the cardiologists and surgeons would never agree to have anything but ACTA anesthesia . Cardiovascular intervention continues to become more and more complex.
One of the other major points to stress is that the current crop of cardiac surgeons and interventional cardiologists are actually playing fair in the sandbox. There are heart teams, structural teams and according to all the society guidelines, SCAI, AHA, ACC, STS, SCA Anesthesiologists have to be on this team. There is never mention of the CRNA. This is mandatory and guideline driven.
The younger surgeons and proceduralists are actually really happy we are there.
As an MD you are on equal footing as any of the proceduralists and really should make that space if that doesn't currently exist in your work setting.
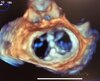
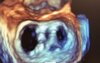
So that being said. I don't mind the anesthesia nurse checking blood or untangling lines in a complex case but there needs to be role clarification and delineation. So when it comes to the procedures: Lines, Intubations, Inductions, art lines, ECMO, Device management, going on and off pump, TEE, TTE, Structural intervention...its on us. And some of the newer bleeding edge topics ECMO Cannulation, ICE, etc. we own this space. But if you want to run the ACT/TEG machine sure..have at it.
What needs to happens is not necessarily define anesthetics based on the presence of a sedative medication (which is basically a continuous level of anesthetic depth) but improve our risk stratification from the current simplistic ASA 1,2,3,4 score.
The ASA needs to improve risk stratification if it really wants the ACT model. So...Instead of some random number put down on the preoperative note, there should be a calculator of 50 variables. Heck we can even feed it a database of 100000 anesthetics which will then help guide anesthesiology coverage schemes.
25 yo healthy gallbladder, Sleeve, and lipoma sure CRNA 1:3.
75 year old triple valve with EF of 15% yeah 1:1.
And sure optho rooms might be usually started 1:3 coverage but every so often the optho room may need 1:2 or 1:1.
The ASA needs to come out and declare the exact things that we do. Not just say hey we do Anesthesia...What the hell does that even mean.
It needs to clearly define everything we should do and things CRNAs should not do. Otherwise, there will always be whack job sell out MDs out there teaching the next anesthesia nurse that walks by how to do a ISB just so they can feel good about themselves and sell the patient and the profession short.